This chapter should be cited as follows:
Dutta A, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.414323
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 11
Labor and delivery
Volume Editor: Dr Edwin Chandraharan, Director Global Academy of Medical Education and Training, London, UK
Chapter
Presentation and Mechanism of Labor
First published: February 2021
Updated: January 2025
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
The mechanism of normal labor involves a series of events that take place in the reproductive tract, allowing the birth of a viable fetus at term; followed by expulsion of the placenta and membranes from the vagina. The World Health Organization defines normal labor as starting spontaneously at term (37 completed weeks of gestation) for a fetus with cephalic presentation, progressing without maternal or fetal complication, and resulting in the delivery of the fetus followed by the placenta and membranes.
The factors that trigger labor at term are not fully understood; however, it is postulated to result from changes in the hypothalamic–pituitary–adrenal axis, increased fetal cortisol levels, and placental enzymatic activity. Complex interactions of hormones between the uterus, placenta and fetus occur. Fetal dehydroepiandrosterone sulfate (DHEAS) is converted to estriol and estradiol by the placenta.1 This potentiates oxytocin receptors in the myometrium, reduces the progesterone/estrogen ratio and upregulates myometrial gap junctions to facilitate uterine contractions. The onset of labor is also associated with an increase in prostaglandin production in the placenta and cervix, further inducing their receptors and facilitating cervical ripening (PGE2) and uterine contractions (PGF2α).2,3,4
A successful normal labor requires coordinated interaction between the maternal pelvis (passage), uterine activity (power) and the fetus (passenger).
MATERNAL PELVIS (PASSAGE)
The maternal pelvis comprises five bones: the sacrum and coccyx posteriorly, an innominate bone on each side and the pubic bone anteriorly. The bones are articulated by four joints: the symphysis pubis anteriorly, two sacroiliac joints posteriorly and the sacrococcygeal joint inferiorly.
The pelvic brim extends from the sacral promontory, along the ilium on each side, and circularly along the ridge, dividing the pelvis into the upper false pelvis and the lower true pelvis. The significance of the false pelvis is to support the pregnant uterus; the true pelvis is a bony passage for the fetus to pass during labor. The true pelvis is shallow anteriorly, formed by the symphysis pubis (4–5 cm), and deep posteriorly, formed by the sacrum and coccyx (10 cm). It is divided into three parts: inlet, cavity and outlet (Figure 1). The pelvic inlet has a wide transverse diameter (approximately 13 cm), the midcavity of the pelvis is round, whilst the outlet has a wide anteroposterior diameter (approximately 11 cm).
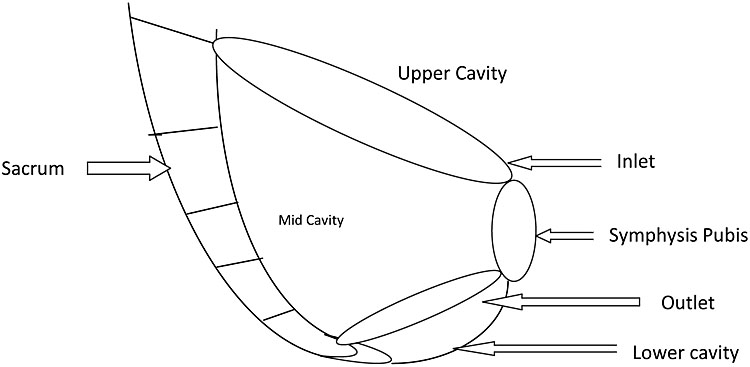
1
Diagram of boundary of pelvic mid cavity.
UTERINE ACTIVITY (POWER)
Uterine contraction is characterized by its intensity, frequency and duration. External tocodynamometry is a qualitative method of measuring uterine activity. It records the frequency and duration of uterine contractions and, when used alongside fetal heart rate monitoring, helps correlate fetal heart rate patterns with uterine contractions.
Quantitative assessment of intrauterine pressure to measure the strength of uterine contraction can be done by placement of an intrauterine pressure catheter (IUPC). This is measured in Montevideo units (MVU). Uterine activity varies in different stages of labor: in the latent phase it is approximately 100 MVUs, in the active phase it is approximately 175 MVUs and in the second stage it is approximately 250 MVUs .5 However, placement of an IUPC is an invasive procedure which is not routinely performed due to lack of evidence of effectiveness and it is likely to be used only when clinically indicated.
FETUS (PASSENGER)
For a successful outcome, the fetal skull, shoulders, trunk and buttocks need to pass through the maternal pelvis. Several variables relating to the fetus influence its journey through the birth canal.
Fetal size
Fetal size can be estimated by palpation and ultrasound scan, and measurements can be assessed by means of a customized growth chart. These methods are subject to a variable degree of error.
Fetal lie
Fetal lie refers to the relationship between the long axis of the fetus and that of the uterus. A fetus in longitudinal lie is suitable for vaginal delivery.
Presentation
Presentation refers to the part of the fetus that directly overlies the lower pole of the uterus or pelvic inlet. In a longitudinal lie, the presentation may be cephalic or breech, while in an oblique or transverse lie, it may involve the shoulders or a compound presentation, in which more than one part overlies the pelvic inlet.
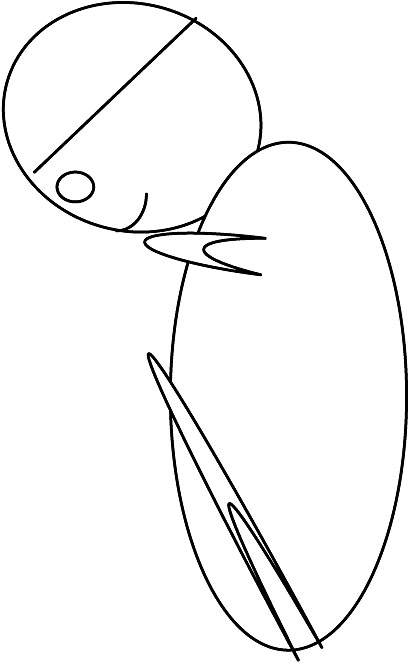
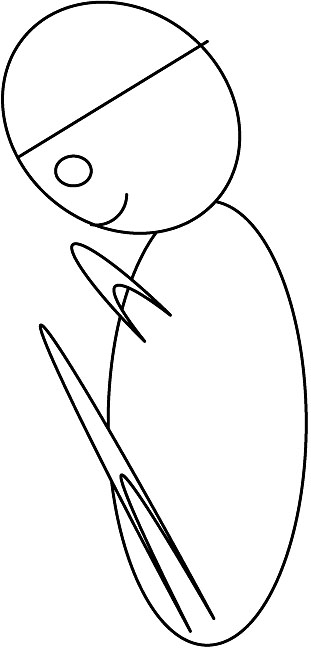
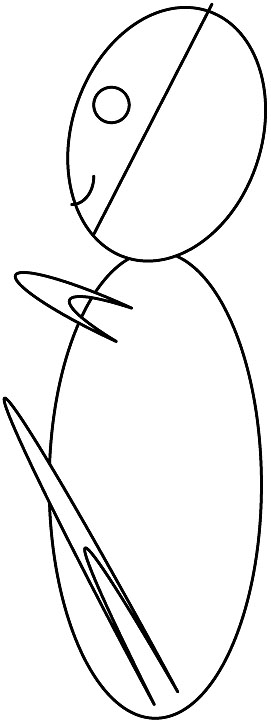
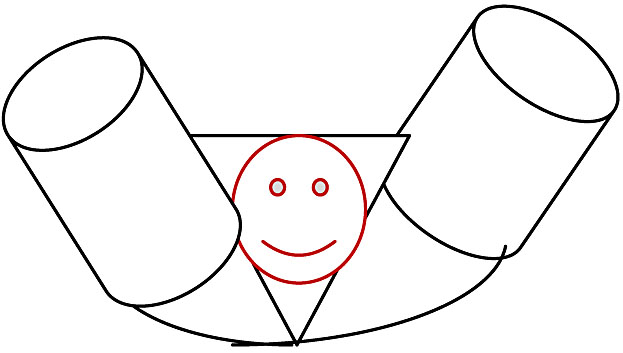
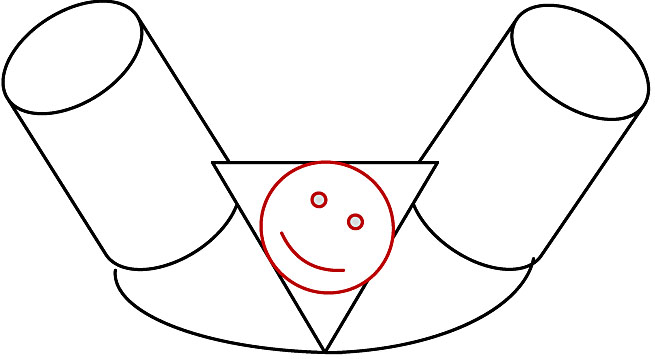
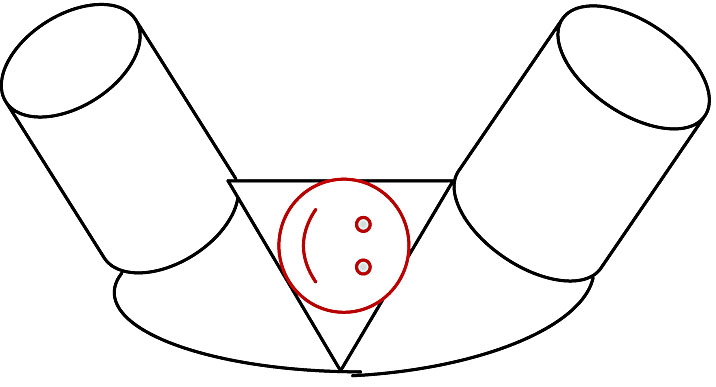
Attitude
Attitude refers to the position of fetal head in relation to the fetal spine (the degree of flexion and/or extension of the fetal head). Flexion of the fetal head is the favored attitude as it presents the smallest diameter to the maternal pelvis (Figures 2–5).
Position
Position refers to the relationship of the presenting part to the maternal pelvis.
2 Diagram showing full flexion of the head with suboccipitobregmatic diameter of 9.5 cm. |
3 Diagram showing deflexed head with suboccipitofrontal diameter of 10 cm. |
4 Diagram showing deflexed head with occipitofrontal diameter of 11 cm. |
5 Diagram of extended head with mentovertical diameter of 13 cm. |
STAGES OF LABOR
Labor is described in three stages:
First stage
The first stage involves onset of regular uterine contractions, progressive effacement and dilatation of the cervix to 10 cm. This stage is divided into the latent and active phases.
The duration of the latent phase may vary from days to weeks in nulliparous women. It is characterized by regular painful uterine contractions, progressive effacement and dilation of the cervix.
The active phase is when cervical dilatation is 4 cm and beyond, in the presence of regular painful uterine contractions.
In nulliparous women, the first stage of labor lasts on average 8–18 hours. In parous women it is usually between 5 and 12 hours.
Second stage
- The stage of labor from full dilatation of the cervix to delivery of the baby is defined as the second stage.
The initial part of the second stage is termed 'passive' and is when there is no voluntary maternal effort. The latter part of the second stage is termed 'active' and is when there is active maternal effort and expulsive uterine contractions to progressively move the presenting part to deliver the baby.
Birth is expected within 3 hours of the start of the active second stage in most nulliparous women and within 2 hours in most parous women.7
Third stage
- The third stage is the time from birth of the baby till expulsion of the placenta and membranes. This is usually completed with 30 minutes of birth following active management or 60 minutes if physiological.
MECHANISM OF NORMAL LABOR
The fetus undertakes a series of movements to adapt the smallest possible diameter of the presenting part to the anatomy of the maternal pelvis. The commonest and optimal situation is the fetus in longitudinal lie, with cephalic position and a well-flexed attitude.
For descriptive purposes, the fetal head is typically used as the reference point, but the trunk also participates in and may initiate some of the movements during labor. These cardinal movements are: (1) engagement; (2) descent; (3) flexion; (4) internal rotation; (5) extension; (6) restitution; (7) external rotation.
Engagement
- Engagement is the mechanism by which the greatest transverse diameter of the fetal head, the biparietal diameter (BPD) (9.4 cm), is at or has passed the pelvic inlet (brim). In nulliparous women, engagement occurs weeks prior to onset of labor, whereas in parous women it may occur in labor.
Descent
- Descent is a continuous process throughout the first and second stages of labor.
Flexion
- The head is already flexed to an extent at the time of engagement but further flexion occurs during the first stage of labor due to soft tissue resistance of the pelvis. Flexion facilitates the shortest anteroposterior diameter, the suboccipitobregmatic diameter (9.5 cm), to be presented at the pelvic outlet.
Internal rotation
- Internal rotation is the turning of the fetal head in such a manner that the occiput gradually moves anteriorly toward the symphysis pubis. This movement aligns the long diameter of the fetal head with the anteroposterior diameter of the pelvic outlet i.e. the longest diameter of the outlet. This shift occurs from the previous occipitolateral position to facilitate passage through the birth canal. During internal rotation, the occiput moves forwards under the pubic arch. The fetal shoulders typically enter the pelvis in the transverse diameter at the pelvic inlet. As the head rotates, the flexibility of the fetal neck allows this movement to occur smoothly.
Extension
- The force of uterine contractions, active maternal effort and the guidance of the pelvic floor muscles facilitate the birth of the head through extension as it passes beneath the pubic arch (Figure 6) . The chin slides over the edge of the perineum and becomes separated from the chest wall i.e. the head becomes extended. The vaginal outlet is stretched and crowning occurs. With progressive distension of the perineum, the occiput, forehead, mouth and chin are delivered successively.
6
Fetal head position at birth by extension.
Restitution
- Restitution (Figure 7) is the visible external movement of the fetal head that occurs to correct the torsion of the neck sustained during internal rotation. The direction of movement is opposite to that of the internal rotation (45°). This allows the head to align with the shoulders. The occiput points toward the maternal thigh ipsilateral to its position before internal rotation.
7
Fetal head restitution.
External rotation
- External rotation (Figure 8) is the movement of the head caused by the internal rotation of the shoulders as they align with the anteroposterior diameter of the pelvic outlet. This movement is visible externally and occurs in the direction opposite to internal rotation but in the same direction as restitution. At this point, the shoulders are positioned in the anteroposterior diameter. The anterior shoulder passes under the pubic arch, while the posterior shoulder sweeps over the perineum. After the shoulders are delivered, the rest of the body is expelled spontaneously through lateral flexion.
8
Fetal head external rotation.
SUMMARY
Labor is a crucial time for the mother and fetus. This is the most perilous journey undertaken by the fetus in utero. For the clinician, it is important to know and identify any deviation from the normal pathway. Despite significant developments in imaging techniques to assist in making the right decision for the patient, in labor management, clinical assessment still plays a key role.
PRACTICE RECOMMENDATIONS
- Precise assessment of onset of labor is crucial to identify any deviation from the normal course.
- The latent phase of labor is when there are painful uterine contractions and some cervical effacement with dilatation up to 4 cm. The duration may vary from days to weeks.
- Progress of the first stage of labor is assessed by progressive cervical dilation at a rate of approximately 2 cm every 4 hours, increasing frequency and intensity of uterine contractions, and progressive descent and rotation of the fetal head.
- There is no substantial evidence to support use of CT or MR imaging in routine pelvic assessment. Imaging may assist in evaluating the pelvis during labor in women with a history of pelvic fracture and thereby help in decision-making regarding their management.
- Monitoring of fetal heart rate should be a routine practice to ensure fetal wellbeing during the process of labor.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Kilpatrick S, Garrison E. Normal labour and delivery Normal and problem pregnancies, 7th edn., 246–9. | |
Makino S, Zaragoza DB, Mitchell BF, Robertson S, Olson DM. Prostaglandin F2alpha and its receptor as activators of human decidua. Semin Reprod Med. 2007 Jan;25(1):60-8. doi: 10.1055/s-2006-956776. PMID: 17205424. | |
Beshay VE, Carr BR, Rainey WE. The human fetal adrenal gland, corticotropin-releasing hormone, and parturition. Semin Reprod Med. 2007 Jan;25(1):14-20. doi: 10.1055/s-2006-956772. PMID: 17205420. | |
Lockwood CJ. The initiation of parturition at term. Obstet Gynecol Clin North Am. 2004 Dec;31(4):935-47, xii. doi: 10.1016/j.ogc.2004.08.012. PMID: 15550343. | |
Caldeyro-Barcia R, Sica-Blanco Y, Poseiro JJ, Gonzalez Panizza V, Mendez-Bauer C, Fielitz C, Alvarez H, Pose SV, Hendricks CH. A quantitative study of the action of synthetic oxytocin on the pregnant human uterus. J Pharmacol Exp Ther. 1957 Sep;121(1):18-31. PMID: 13481824. | |
Miller F. Uterine activity, labor management, and perinatal outcome. Semin Perinatol. 1978 Apr;2(2):181-6. PMID: 734452. | |
Intrapartum guideline NICE nice.org.uk (CG190). |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards programme CLICK HERE)