This chapter should be cited as follows:
Centini G, Cannoni A, et al., Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.420273
The Continuous Textbook of Women’s Medicine Series – Gynecology Module
Volume 8
Gynecological endoscopy
Volume Editors:
Professor Alberto Mattei, Director Maternal and Child Department, USL Toscana Centro, Italy
Dr Federica Perelli, Obstetrics and Gynecology Unit, Ospedale Santa Maria Annunziata, USL Toscana Centro, Florence, Italy
Chapter
Surgical Anatomy of the Pelvis
First published: September 2023
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
The anatomy of the pelvis can be illustrated in several different way, accordingly to what we need it for; it can be surgical, functional, topographical, or either defined by the specific component such as neuro or vascular anatomy of a specific organ.
Anatomy has been studied since the 14th century, but the recent introduction of minimally invasive surgery allowed the anatomists to study it in live tissue with magnification providing a new insight.
The aim of this chapter is to provide all the basic knowledge of anatomical structures in the pelvis to perform basic surgical procedure, including tips and tricks on how to use the anatomy to open the pelvic spaces and to locate relevant structures that must be spared.
MUSCLES AND FASCIAS OF THE PELVIS
Muscles
The central muscular element of the pelvis is represented by the pelvic floor (or pelvic diaphragm), consisting of levator ani muscle and coccygeus muscle, covered by pelvic fascia.1 Levator ani muscle consists of three different parts: the pubococcygeus; the iliococcygeus; and the puborectalis.
The pelvic floor has two hiatuses: (1) anterior urogenital hiatus, through which the urethra and vagina pass through; (2) the posterior rectal hiatus, through which the anal canal passes. The pelvic floor divides the pelvic cavity from the perineal region, which is located caudally.
The pelvic floor is extremely important in providing sustain for pelvic organs and in providing urinary and bowel continence, being part of the urinary and anal sphincters.2
The pubococcygeus muscle, shaped like a hammock, is the main component of levator ani muscle and arises from the pubic bone and is directed dorsally towards the coccyx. Some of its fibers are directed towards the urethra and the vagina. The puborectalis muscles arise from the lower part of the pubic symphysis and run caudally and dorsally to conjoin behind the anorectal junction, forming a muscular sling. The iliococcygeus muscle represents the dorsal and lateral part of levator ani muscle; it arises from the ischial spine and is directed towards the lower segment of the coccyx.
The coccygeus muscle is located dorsally to the levator ani muscle stretching from the caudal margin of the ischial spine to the lateral margins of the sacrum and of the coccyx.
Another important muscle of the pelvis is represented by internal obturator muscle, which originates from the pubic rim, the obturator membrane and from the ischium near the membrane.3 It exits the pelvis passing through the lesser sciatic foramen, and inserts on the greater trochanter of the proximal femur; with some of its fibers, it helps to support urinary bladder. The pelvis is delimited dorsally and laterally by piriformis muscle, a flat and pyramidally shaped muscle, which originates from the ventral surface of the sacrum, and the superior margin of the greater sciatic notch and exits the pelvis passing through the greater sciatic foramen and inserts on the greater trochanter. Piriformis muscle is an important anatomic landmark, because it divides the greater sciatic foramen in two parts: superior and inferior.
The elevator ani muscle has a funnel shape, partially shifted ventrally where the vaginal and anal hiatus open. This area is the weakest of the pelvic floor and can be exposed to prolapse.4 The puborectalis has the role to constrict the vagina and the rectum against the pubis to close the hiatus during Valsalva maneuver to reduce the exposure of this region to the abdominal pressure.
However, to reinforce this area a fibro-muscular structure called urogenital diaphragm is locate behind the pelvic floor in the anterior part of the perineum.
The urogenital diaphragm consists of two different muscles, which are the deep transverse muscle of the perineum and the external sphincter muscle of the urethra, and a fascial component (superior and inferior fascia of the urogenital diaphragm). The urogenital diaphragm is delimited by a muscular-aponeurotic lamina, which has a triangular form; in females, the vagina and urethra pass through the urogenital diaphragm.
Fascias
In the pelvis two different fascial systems can be identified: the one formed by pelvic parietal fascia, and the one formed by pelvic visceral fascia. Pelvic parietal fascia covers muscular and bone structures, which delimit the pelvic cavity and others (hypogastric vessels, sacral plexus). The fascia adheres firmly to the periosteum and to the muscles and it forms a reflection on the surface of pelvic organs, covering and fixing them to the pelvic walls. The pelvic parietal fascia adheres to the ventral surface of the sacrum and of the coccyx, and at that level it is called pre-sacral fascia; it covers also the piriformis muscle, at that level being called hypogastric fascia. The pelvic visceral fascia covers the surface of pelvic organs and it is not uniformly distributed, being more thick on the junctional areas of pelvic organs, where it forms longitudinal or transversal branches of connective tissue, which maintain pelvic organs separated from each other. The pelvic visceral fascia is formed by two leaflets and, as well as covering the surface of pelvic organs, it covers also the ligaments of the parametrium (round ligament, uterosacral ligament, cardinal ligament, uteroovarian ligament, infundibulopelvic ligament); pelvic visceral fascia also forms the peritoneal plications, which are found in the space between pelvic organs (e.g., mesosalpinx, mesovarium, parts of the broad ligament).
The connective tissue included between pelvic parietal fascia and pelvic visceral fascia, the so-called extra-serous pelvic fascia, contains the nervous and vascular support needed by pelvic organs.
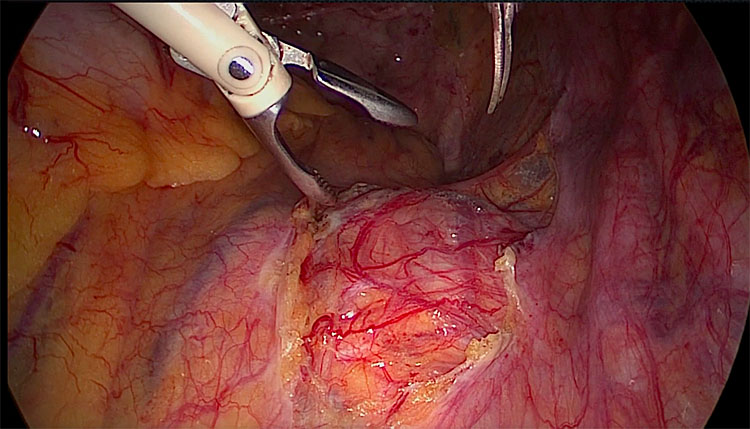
The pelvic fascia is not represented uniformly and it becomes stronger when covering the vagina forming the so-called pubo-cervical fascia anteriorly and the rectovaginal fascia posteriorly (Figure 1).
1
Laparoscopic development of the vesicovaginal space. The pubocervical fascia (below) is the dense whitish tissue covering the vagina, separated by the bladder anteriorly (above).
These two structures are not dissectible from the vagina itself without sharp instruments and play a role in preventing pelvic organ prolapse.
The pubo-cervical fascia stretches from the pubis ventrally and the ischiatic spine dorsally and finds its lateral attachment on the levator ani muscle forming the arcus tendinous fascia pelvis.
Defect of these fascia are the main cause or anterior and posterior compartments' prolapse.
Ligaments
Ligaments are structures that connect the midline organs to the pelvic side wall providing an extra help to muscles and fascias in suspending the pelvic organs.
Those of gynecological interest inside the pelvis are four: the round ligament, the uterosacral ligament, the cardinal ligament (or paracervix), and the infundibulopelvic ligament.
The round ligament is a structure made of dense connective tissue, which is found between the uterine cornua and the inguinal canal. It is comprehended between the anterior and posterior leaflets of the broad ligament and is not a proper ligament but a reflection of the peritoneum. The round ligament has essentially a function of suspension in orthostatism.
The uterosacral ligaments are two structures attached ventrally to the uterine torus and that run in a dorso-lateral direction to disappear in the loose connective tissue of the retroperitoneal space, without a real connection to sacrum itself.5 The role of this structure is the suspension in orthostatism and close to their origin from the uterus they run in close contact with the hypogastric nerve and the ureter.
The cardinal ligament has the more complex anatomy of all the other pelvic ligaments: it is located laterally to the uterus and the vagina covered by the puborectal fascia ventrally and the rectovaginal fascia dorsally.
This structure provides attachment of the upper vagina and the cervix to the pelvic side wall following the path of the hypogastric artery preventing apical prolapse.
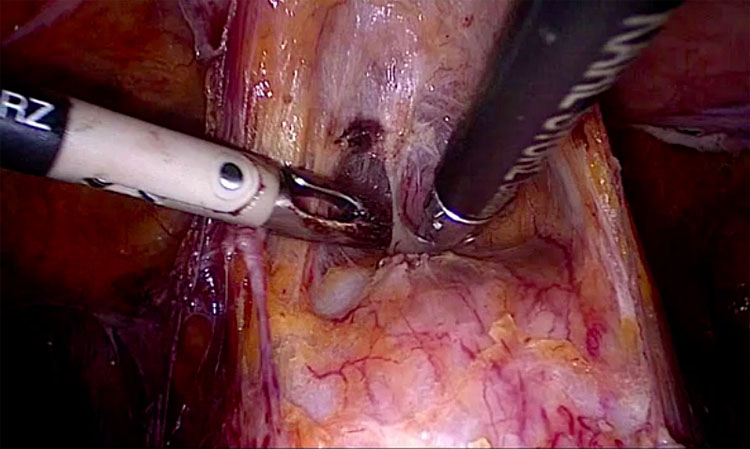
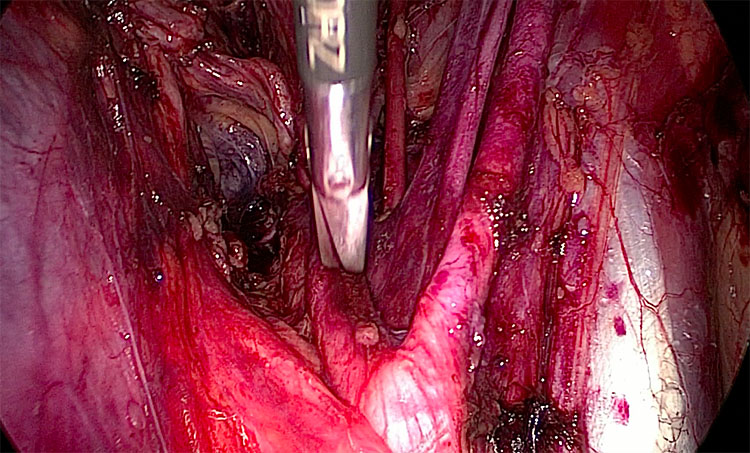
The cardinal ligament, as it was historically called (now being called “paracervix”) comprehend several structures of interest for gynecological surgery, and in its medial part it creates a tunnel to let the ureter join the bladder (Figure 2).6
2
Right side. The uterine artery runs with a lateromedial direction towards the uterus, crossing the ureter.
At the top of this ligament is located the uterine artery with the superficial uterine vein that can be used as a landmark to identify the ligament. Immediately below the uterine artery, the ureter enters the canal passing above the deep uterine vein. The deep uterine vein is an important landmark to identify the nerve bearing area of the cardinal ligament.
The caudal part of the ligament below the deep uterine vein comprehends fibers of the inferior hypogastric plexus and a surgical damage of this area can cause dysfunction to the pelvic organs, especially bladder voiding problems.7
It is of the utmost importance for the gynecologist and for all the other health providers to comprehend the anatomy of the female pelvis to orientate the diagnosis and the surgical treatment of all the pathologies that can occur in this anatomic region.
The ureter
The ureter is one of the longest organ in the human body and probably one of the least vascularized and should be handled with care. Approximately 70% of ureteral injuries occur during gynecological procedures and most of them are recognized postoperatively.8
A precise knowledge of ureteral anatomy and of its pathway can play a pivotal role for a gynecological surgeon transforming this structure from an enemy to an important surgical landmark.
The ureters are two tubes that run from the kidney all the way down to the bladder with a path long between 20 and 30 cm and with a diameter of 3–4 mm.
The lumen of the ureter is around 2 mm, coated with urothelium surrounded by the muscle coat, which is responsible for the bilateral alternating peristaltic movements of the ureter (at a velocity of 2–3 cm/s). In cross section, the bundles form two muscle layers fused by connective tissue. The inner layer is mainly longitudinal in arrangement, and in the outer layer the muscle bundles are arranged circularly. Near the bladder the intrinsic musculature is separated from a third layer, the muscular layer of Waldeyer; it consists of longitudinally arranged muscle bundles, which emerge from the bladder wall into the ureter.
The ureter path can be dived in an abdominal and in a pelvic segment.
In its abdominal part the ureters descend on top of the psoas muscle to reach the pelvic brim crossing the iliac arteries to enter in the pelvis. Starting from the iliac arteries the pelvic segment of the ureter can be divided into five segments:
- The parietal segment that passes over the iliac artery.
- The retro-ligamental part where the ureter runs retroperitoneally and can be seen in transparency in the lateral side wall.
- The intra-ligamental part where the ureter enters into the ureter channel passing under the uterine artery, becoming invisible to the surgeon.
- The retro-vesical part, when the ureter joins the bladder passing between the cranial and caudal leaf of bladder’s pillars.
- The vesical part, when it runs inside the bladder’s wall.
At the beginning of its path in the pelvis the ureters run on the pelvic side wall parallel to the uterine artery laterally to the pararectal fossa and then, approaching the parametrium, they turn ventrally to enter the ureteral tunnel just under the uterine artery.
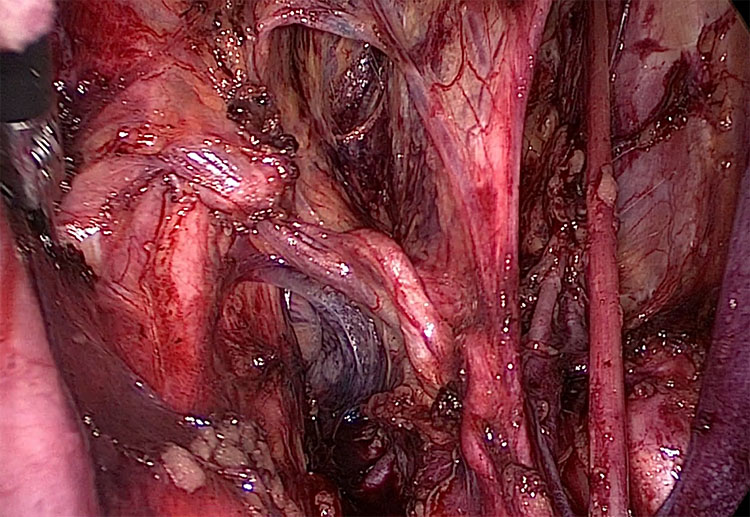
After entering the ureteral tunnel the ureters run in the medial part of the paravesical fossa covered by the anterior paracervix dividing the paravesical fossa from the vesicovaginal space (Figure 3).
3
Right side. Medial dissection towards the retrovesical portion of the ureter. The uterine artery is lateralized to visualize the paracervix.
Blood and nerve supply
The arteries, which supply the ureter, can vary along its pathway in the abdominal cavity, being no more than 4–5, arising from the renal arteries, common iliac arteries, abdominal aorta and gonadal arteries, while for the lower third of the ureter the supply can be variable, and in women it receives branches from the uterine and vaginal arteries.
These arteries create an anastomotic network inside the adventitia layer, which means that the occlusion of a single vessel does not compromise the blood supply of the ureter. The adventitia also contains the ureteric plexus, that receives nerve fibers from the renal plexus and from aortic plexus in its upper part, while the middle part receives branches from the superior hypogastric plexus and the lower part receives branches from the lower hypogastric plexus. The sensation is provided to the ureters from T11–L2 segments of the spinal cord and the pain arising of these organs is generally referred to the flank and upper part of the front of the thigh.
NERVES AND VESSELS OF THE PELVIS
Blood supply of the pelvis
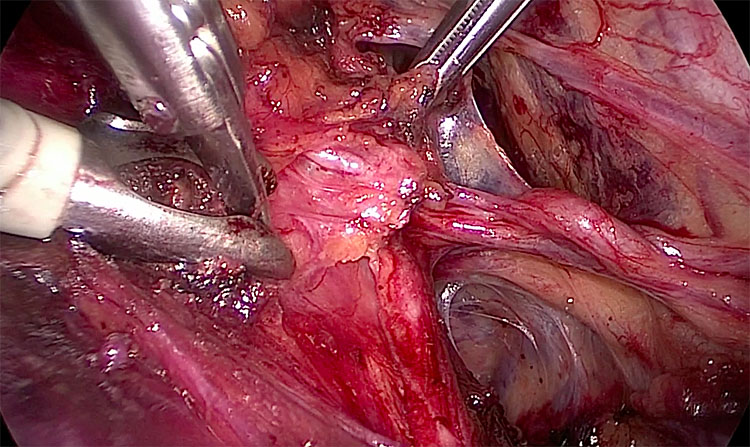
The abdominal aorta, the main human body vessel, slightly overlies the inferior vena cava with a mild left positioning. It bifurcates at the level of the fourth lumbar vertebrae below the level of the umbilicus into the right and left common iliac arteries.9 The anatomical knowledge of this area is of paramount importance for a cautious entry during primary trocar insertion at the level of the umbilicus that is located around 5 cm above the bifurcation. According to Sandadi et al., injury to major retroperitoneal vessels occurs in 0.3 to 1% of the cases during primary trocar entry.10 The inferior vena cava satellites the aorta, bifurcating above the promontory into right and left common iliac veins but with slight lateralization to the right. The left common iliac vein is located immediately caudal to the aortic bifurcation, just above the promontorium. The left common iliac vein is an important landmark during promontory dissection for sacrocolpopexy procedure and must be identified at the beginning of the dissection.11 From the vena cava and the aorta arise the middle sacral vein and artery that run over the sacrum beyond the presacral fascia. In this area all these structures are covered by the presacral fascia and have a strict relationship with the superior hypogastric plexus that is located over the aorta. From the superior hypogastric plexus arise two main nerves, the right and left hypogastric nerve. The hypogastric nerves run on the pelvic side wall just beyond the peritoneum and bring the sympathetic innervation to the inferior hypogastric plexus (Figure 4).
4
The right hypogastric nerve is the tense structure visibile after dissection of the promontorium, arising from the superior hypogastric plexus.
With an average length of 5 cm, the common iliac artery divides into internal and external iliac artery at the level of the sacroiliac joint. To note, the external iliac artery has no branches in the pelvis, and before leaving it, it gives the circumflex and the inferior epigastric arteries that run under the peritoneum of the anterior wall in a medial direction.
The external iliac vein follows the pathway of the artery with a slight medial position and at the level of the cooper, ligament, just before leaving the pelvis, it gives the origin of the corona mortis vein, that anastomoses with the obturator vein, creating a circle between the external and the internal iliac veins. This small vein can be scarified without any consequences, but it is important to localize it during pelvic lymphadenectomy to avoid massive hemorrhage.
The internal iliac artery usually measures around 3–4 cm before it divides into a posterior and anterior trunk. The posterior trunk branches into the iliolumbar, lateral sacral and superior gluteal branches. These branches of the posterior trunk supply the pelvic wall and the gluteal muscles with the superior gluteal artery. During major pelvic hemorrhage, such as a post-partum one, it is important to spare the posterior truck ligating the hypogastric artery 3 to 4 cm below its bifurcation, in order to avoid gluteal muscle ischemia. The anterior trunk has nine branches, three of which supply the muscles: obturator, internal pudendal, and inferior gluteal. The rest of them supply the pelvic organs: uterine, superior vesical, vaginal, and middle rectal arteries.
The obturator artery is the first division and the only lateral branch going in the paravesical space irrigating the internal obturator muscle, being satellite of the obturator vein. This artery lies on the lateral part of the paravesical space and exits the pelvis trough the obturator foramen.
As the second division of the anterior trunk, the umbilical, the uterine and the superior vesical arteries arise with a common origin in the majority of cases. This anatomical peculiarity gives to the umbilical artery a pivotal role as the main landmark to approach the paravesical space, making a peritoneal fold dividing the paravesical space into medial and lateral.
The uterine artery moves medially with a tortuous path on top of the paracervix to join the uterus at its lateral walls followed by the superficial uterine vein. The common origin with the umbilical artery plays a role to locate this artery in the retroperitoneal space.
The umbilical artery can be clearly identified on the ventral side of the abdominal wall and proceeding with a dissection in a ventro-dorsal direction and remaining medial to it, the umbilical artery lead the surgeon to the uterine artery.
Another important landmark is the deep uterine vein, that is located in the paracervix just below the ureter. This anatomical landmark highlights the nerve baring area of the paracervix.
Moving caudally, the middle rectal artery arises from the internal iliac artery going medially to bring blood supply to the rectum, it crosses in the pararectal space piercing the inferior hypogastric plexus. Thus, it represents an important landmark to locate the inferior hypogastric plexus and to avoid rectal functional damage during endometriosis surgery.12
The terminal branch of the internal iliac artery is the pudendal artery that leaves the pelvic through the inferior piriformis foramen after the origin of the inferior gluteal artery.
The pudendal artery passes just beyond the sacrospinous ligament to enter the Alcock channel that drives this artery, along with the homonymous vein and nerve, to the perineum.
The ovarian arteries originate from the aorta and run through the retroperitoneal space reaching the pelvic brim lateral to and above the ureter, thus suspending the ovary with the infundibulopelvic ligament. However, the ovarian veins drain the ovaries and run parallel to the ovarian artery with a slight difference, draining into the inferior vena cava at the right side and into the left renal vein on the left side.
Pelvic nerves
Pelvic innervation can be divided in a somatic and in an autonomic on; this system is very complex at it gives innervation to the lower abdomen and to the legs, and provides also autonomous function to the whole pelvic viscera.
The inferior hypogastric plexus is a nerve network that comprehends both sympathetic and parasympathetic components. The sympathetic fibers join the plexus through the hypogastric nerve that originates from the superior hypogastric plexus and also from the lateral sympathetic chain. The parasympathetic component joins the plexus through the pelvic splanchnic nerves, that are thin fibers arising from S1 to S3.
The plexus is located on the lateral and medial aspect of the pararectal fossa, below the level of the deep uterine vein, and it dives into three different components to give nerve supply to the rectum, uterus, and bladder.
The genitofemoral nerve (L2–L4) runs on the anterior aspect of the psoas muscle. Injury can be due to pelvic lymphadenectomy and ureteral re-implantation as well as pressure from an orthostatic retractor (Figure 5). Its injury can cause pain, paresthesia in the inguinal fold, labia majora, and the medial thigh. Whilst the lateral cutaneous nerve lies over the iliacus muscle, and its compression can be either caused by retractors or excessive flexion of the hip, thus leading to paresthesia over the anterior and lateral thigh.
5
Right side view after pelvic lymphadenectomy. The genitofemoral nerve is the translucent linear band which runs medio-lateral lying on the psoas muscle.
The femoral nerve (L2–L4), is the largest branch of the lumbar plexus, emerging from the inferolateral surface of the psoas muscle, it runs under the inguinal ligament, providing mainly innervation to the anterior thigh. Its injury due to thigh hyperflexion with excessive hip abduction might lead to inability to flex the thigh and extend the knee.
The obturator nerve (L2–L4), runs from the lumbar plexus into the true pelvis and exits through the obturator canal to supply mainly the adductor muscles and skin over the inner thigh. It may be injured during pelvic lymphadenectomy at the level of the common iliac vein bifurcation. Similarly, obturator nerve injury usually occurs during TOT procedures. If injured, the patient would end up with a thigh adduction deficit and sensory loss of innervation over the inner thigh.13
The pudendal nerve (S2–S4) originates from the sacral plexus, follows the pudendal artery along its course, leaves the pelvis through the greater sciatic foramen and passes under the sacrospinous ligament to join the perineum through the Alcock channel.14 15 Pudendal nerve entrapment usually occurs during sacrospinous fixation, especially if the suture is taken at its proximal part, thus care must be taken during such procedures.14,15
The origin of the sciatic nerve is from the anterior division of L4–S3. It runs caudally to exit the pelvis from the greater sciatic foramen, thus entering into the gluteal region. Though infrequently, it still can be entrapped during gynecological procedures, in particular, placing sutures during sacroiliac fossa hemorrhage. Stretch injury, especially due to wrong patient positioning during surgery (lithotomy position via hip hyperflexion), can lead to hamstring weakness and absent Achilles reflex, along with severe posterior leg pain syndrome, also known as sciatica.
A special concern to the pudendal nerve, the sciatic nerve must be considered in the case of deep endometriosis involving the lateral parametrium, and anatomy is the key to free these nerves.
Pelvic spaces
The pelvic spaces are peritoneal depressions formed by reflections of the peritoneum between organs and pelvic side walls. They are created through the occupation of the peritoneum of the empty pelvic cavities during organogenesis.
Indeed, pelvic spaces are virtual spaces, since they are developed during surgical dissection to access retroperitoneal organs by dividing the peritoneal folds. They are mostly avascular, filled with fatty or loose areolar connective tissues.16
They represent useful anatomical landmarks in order to perform a safe pelvic surgery and to expose anatomical boundaries for specific surgical procedures.17
The pelvic spaces are divided into midline (unilateral) and bilateral spaces, developing on the middle sagittal plane of the pelvis and between this plane and the pelvic side wall, respectively. In an anteroposterior direction, the midline spaces can be listed as follows: the prevesical space, the vesicovaginal space, the rectovaginal space, and the retrorectal or presacral space. The lateral spaces are symmetrical in both the hemipelvis and can be listed as follows: pararectal spaces, paravesical spaces.18
The midline spaces are more frequently used for benign diseases, whereas the lateral spaces are dissected for oncological purposes or for deep endometriosis.
Midlines spaces
Prevesical space – the Rezius space
The prevesical space or Retzius space is an extraperitoneal space located anteriorly in the pelvis between the umbilicovesical fascia,19 and the transversalis fascia of the abdominal wall and the pubic symphysis. It surrounds ventrally and laterally the urinary bladder. Laterally it communicates with the paravesical spaces and inferiorly its boarded by the pubovesical ligaments. Dissection of this space is useful for urogynecological surgery, bladder endometriosis, advanced stage cancers, and drainage of hemorragic fluid collections.
The Retzius space is divided from the abdominal cavity by the peritoneum and more ventrally by prevescical fascia.
Vesicovaginal space
The vesicovaginal space is enclosed between the vagina and the bladder and is developed during any standard hysterectomy. The space can be fully dissected leading to an avascular triangular-shaped space with the apex located at the caudal end of the bladder trigone and laterally limited by the superficial vascular layer of the vesicouterine ligaments.20 Some authors consider vesicocervical and vesicouterine spaces in continuation with the vesicovaginal space along its longitudinal axis.
Rectovaginal space
By accessing through the peritoneal fold covering the pouch of Douglas down to the levator ani muscle, the rectovaginal space can be dissected. Its anterior boundary is the posterior wall of the vagina. Posteriorly the anterior wall of the rectum represents its dorsal limit. Laterally it is enclosed by the uterosacral ligaments and by the rectal pillars. The rectovaginal space is useful in cases of deep endometriosis or cervical cancer and its entrance is located 2 cm below the insertion of the uterosacral ligament on the torus uterinus.21
Retrorectal space
Also known as presacral space. It is limited ventrally by the rectum, dorsally by the sacrum, laterally by the hypogastric fascia. In a cranio-caudal direction, the dissection starts from the peritoneal rectosigmoid junction and finishes at the pelvic floor.22
There is no literature concordance on the fascial system definition of this space but at this level we can identify two anatomical planes, the interfascial plane and the presacral area. In this area we can find two different fasciae, the fascia propria recti, that envelopes the mesorectum and the rectum, whereas the presacral fascia is a layer that covers the promontory and the hypogastric nerves. The inter-fascia layer is the one located between the fascia propria recti and the presacral fascia and is an avascular plane that can be used for rectal resection or presacral neurectomy. While the presacral area is located beyond the presacral fascia (tod’s fascia) and for gynecological surgery the space is opened only at the level of the promontorium during sacropexy.
Lateral spaces
Paravesical space
The paravesical space is enclosed by the bladder medially, the pelvic wall laterally, the pubis anteriorly. The posterior border is the paracervix, which crosses transversally the lateral spaces and divides the paravesical spaces ventrally from the pararectal spaces dorsally.
The obliterated umbilical artery divides the space into a medial and lateral portion. The lateral portion is dissected for oncological purposes, particularly for pelvic lymphadenectomy where the lateral limit of this space, the obturator muscle, must be identified with the obturator nerve and vessels up to their entrance in the obturator foramen. The medial paravesical space is useful in cases of adhesions between the bladder and the uterus during hysterectomy, and for ureteric reimplantation. While the lateral paravesical space is avascular, the medial space is crossed by superior vesical vessels.23
Pararectal space
It is bounded medially by the rectum, laterally by the internal iliac artery, anteriorly by the paracervix and posteriorly by the pelvic wall. Craniocaudal dissection starts from the posterior leaf of the broad ligament and terminates at the pelvic floor.
The pararectal space dissection can be divided into a medial or lateral component accordingly to the ureter location.
The medial part of pararectal space (medial to the ureter) – also known as Okabayashi’s space – has an important role in preserving the nervous component of the pelvis because it is at this level the ureter, the uterosacral ligament and hypogastric nerve, are in close contact. The development of this space allows the identification of the nerve. On the lateral aspect of the pararectal fossa is located the inferior hypogastric plexus. This plexus is inconstantly crossed by the middle rectal artery, which is the only vascular structure of this space. The middle rectal artery and its surrounding tissues are also defined as the lateral ligament of the rectum.24
The lateral pararectal space – also known as Latzko’s space – can be developed laterally to the ureter. Latzko’s space dissection allows identification of hypogastric plexus and nervous sacral roots. The vascular component is more represented, with the possibility to isolate the hypogastric artery, the anterior and posterior trunk, and their branches.
The medial part can be dissected for deep endometriosis or sacropexy, ureteric and nervous fibers isolation and injury prevention, while the lateral pararectal space is exposed for oncological purposes.25
Iliolumbar space
It is located between the common iliac vessels medially and the psoas muscle/pelvic side wall laterally, and it is of upmost importance for its dense nerve components.
Inside the iliolumbar fossa the lumbosacral trunk originates from the lumbar plexus covered by lumbosacral vessels and joins some nerve fibers from the sacral plexus to give the sciatic nerve directed inside the infrapyriformis canal. The superior gluteal nerve is the only branch of the lumbosacral trunk, exiting from the suprapyryformis foramen along with the superior gluteal artery and vein. The obturator nerve is more superficial and medial, whereas the pudendal nerve is more caudal and lateral.26
The iliolumbar space is dissected mostly in cases of pudendal neuralgia, pelvic side wall endometriosis, and intraoperative nerve mapping (called LANN technique) for functional nervous purposes.
Yabuki’s space
Also called the fourth space, it is essential for nerve-sparing in radical hysterectomy. The Yabuki’s space is placed between the prevesical portion of the ureter and the vagina medially.
To locate and dissect this space, the surgeon must dissect the vesico-vaginal plane and then move laterally toward the vesico-uterine ligament. The dissection of this space allows identification of the ureter in its prevesical component and lateralization and isolation of the nerve bearing part of the anterior paracervix.27
PRACTICE RECOMMENDATIONS
- The knowledge of pelvic surgical anatomy is mandatory for healthcare professionals. To orientate during surgeries, dissection of the pelvic spaces is recommended. Pelvic spaces are virtual spaces developed during surgical procedures, formed by reflections of the peritoneum between the organs and the pelvic walls.
- The pelvis is vascularized by branches of the internal iliac artery or hypogastric artery since the vessels arising from the external iliac artery feed only extrapelvic tissues. The hypogastric artery bifurcates in an anterior trunk and posterior trunk.
- The uterine artery is the most important vessel for the gynecologist. It rises mainly from the hypogastric artery and give supply to the uterus. It crosses over the ureter along its course. It is a landmark to distinguish the lateral spaces, the paravesical and the pararectal.
- The ureter can be divided in 5 segments during its course in the pelvis: parietal, retroligamentar, intraligamentar, retrovesical and vesical segment. As an anatomical landmark, the ureter divides the pararectal space into a medial and a lateral part, before joining the bladder passing through the medial paravesical space.
- The hypogastric nerves and the pelvic splanchnic nerves give the main sympathetic and parasympathetic components of the inferior hypogastric plexus, respectively. The fibers emerging from the inferior hypogastric plexus innervate the urogenital tract and the inferior part of the rectum.
- The central muscular element of the pelvis is represented by the pelvic floor, consisting of levator ani muscle and coccygeus muscle, covered by pelvic fascia. The pelvic floor has two hiatuses, the anterior urogenital hiatus and the posterior rectal hiatus. The pelvic floor is extremely important in providing sustain for pelvic organs and in providing urinary and bowel continence, being part of the urinary and anal sphincters.
CONFLICTS OF INTEREST
Author(s) statement awaited.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
De Lancey JOL. The anatomy of the pelvic floor. Curr Opin Obstet Gynecol 1994;6(4):313–6. | |
Miller Ashton JA, De Lancey JOL. Functional anatomy of the pelvic floor. Ann N Y Acad Sci 2007;1101:266–96. | |
Němec M, Horčička L, Krofta L, et al. Anatomy and biomechanic of the musculus levator ani. Ceska Gynekol 2019;84(5):393–7. | |
De Lancey JOL. Size of the urogenital hiatus in the levator ani muscles in normal women and women with pelvic organ prolapse. Obstet Gynecol 1998;91(3):364–8. | |
DeLancey JOL. Whatʼs new in the functional anatomy of pelvic organ prolapse? Current Opinion in Obstetrics and Gynecology 2016;28(5):420–9. | |
Eid S, Iwanaga J, Oskouian RJ, et al. Comprehensive Review of the Cardinal Ligament. Cureus 2018;10(6):2846. | |
Querleu D, Cibula D, Abu-Rustum NR. Update on the Querleu–Morrow Classification of Radical Hysterectomy. Annals of Surgical Oncology 2017;24(11):3406–12. | |
Ostrzenski A, Radolinski B, Ostrzenska KM. Review of laparoscopic ureteral injury in pelvic surgery. Obstet Gynecol Surv 2003;58(12):794–9. | |
Handa VL, Van Le L. Te Linde’s Operative Gynecology 12th edn. 2019. | |
Sandadi S, Johannigman JA, Wong VL, et al. Recognition and management of major vessel injury during laparoscopy. J Minim Invasive Gynecol 2010;17(6):692–702. | |
Manodoro S, Werbrouck E, Veldman J, et al. Laparoscopic Sacrocolpopexy. Facts Views Vis Obgyn 2011;3(3):151–8. | |
Yoham AL, Bordoni B. Anatomy, Abdomen and Pelvis, Inferior Hypogastric Plexus. Treasure Island (FL): StatPearls Publishing, 2022. | |
Yoshida T, Nakamoto T, Kamibayashi T. Ultrasound-Guided Obturator Nerve Block: A Focused Review on Anatomy and Updated Techniques. Biomed Res Int 2017;2017:7023750. | |
Kaur J, Leslie SP, Singh P. Pudendal Nerve Entrapment Syndrome. Treasure Island (FL): StatPearls Publishing, 2022. | |
Aydogmus S, Kelekci S, Aydogmus H, et al. Obturator nerve injury: An infrequent complication of TOT procedure. In: Aydogmus S, Keleci S (eds) Case Rep Obstet Gynecol 2014;2014:290382. | |
Puntambekar S, Manchanda R. Surgical pelvic anatomy in gynecologic oncology. International Journal of Gynecology & Obstetrics 2018;143:86–92. | |
Ianieri MM, Raimondo D, Rosati A, et al. Impact of nerve-sparing posterolateral parametrial excision for deep infiltrating endometriosis on postoperative bowel, urinary, and sexual function. International Journal of Gynecology & Obstetrics 2022;159(1):152–9. | |
US et al. Functional outcomes of nerve-sparing laparoscopic eradication of deep infiltrating endometriosis: a prospective analysis using validated questionnaires. Arch Gynecol Obstet 2018;298(3):639–47. | |
Cosma S, Ferraioli D, Mitidieri M, et al. A simplified fascial model of pelvic anatomical surgery: going beyond parametrium-centered surgical anatomy. Anat Sci Int 1234;96:20–9. | |
EA et al. Laparoscopic Nerve-Preserving Sacropexy. J Minim Invasive Gynecol 2017;24(7):1075–7. | |
Donnez O. Conservative Management of Rectovaginal Deep Endometriosis: Shaving Should Be Considered as the Primary Surgical Approach in a High Majority of Cases. Journal of Clinical Medicine 2021;10:5183. | |
Melo MG, et al. Pelvic anatomy in laparoscopic surgery for pelvic organ prolapse: dissect your success. Facts Views Vis Obgyn 2022. | |
Mirilas P, et al. Surgical anatomy of the retroperitoneal spaces part II: the architecture of the retroperitoneal space. Am Surg 2010. | |
Ercoli A, et al. Terminologia Anatomica versus unofficial descriptions and nomenclature of the fasciae and ligaments of the female pelvis: a dissection-based comparative study. Am J Obstet Gynecol 2005. | |
Vercellino G, et al. Laparoscopic temporary clipping of uterine artery during laparoscopic myomectomy. Arch Gynecol Obstet 2012;286(5):1181–6. | |
Possover M, Baekelandt J, Flaskamp C, et al. Laparoscopic Neurolysis of the Sacral Plexus and the Sciatic Nerve for Extensive Endometriosis of the Pelvic Wall. min – Minimally Invasive Neurosurgery 2007. | |
Fuji S, et al. Precise anatomy of the vesico-uterine ligament for radical hysterectomy. Gynecol Oncol 2007. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards programme CLICK HERE)

