<< back to Pathology Atlas menu
Pathology Atlas: Uterus
Normal
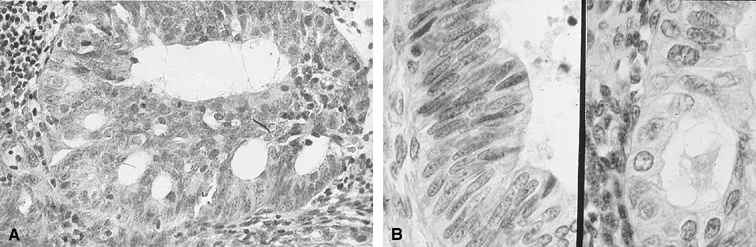
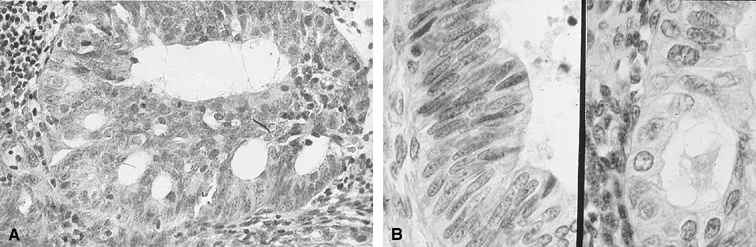
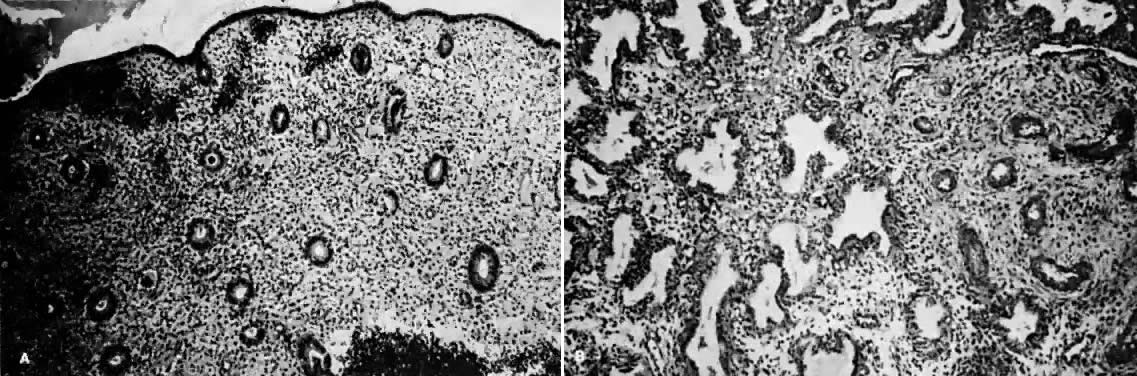
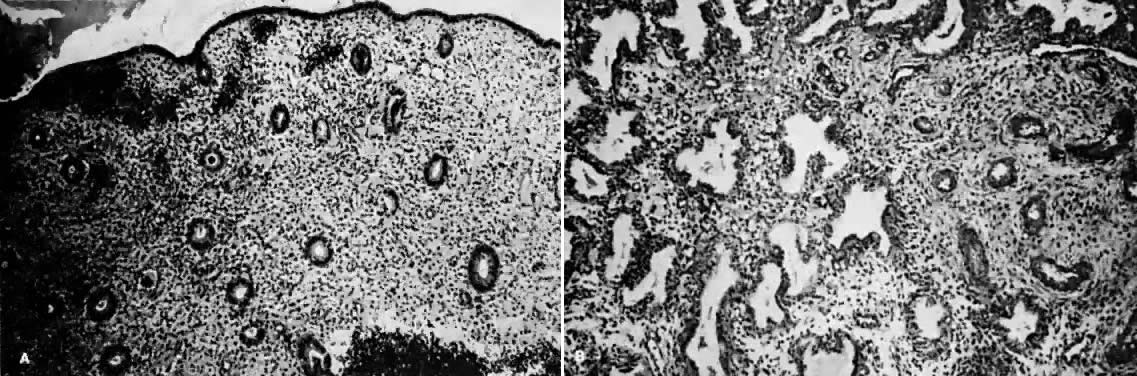 A. Early proliferative endometrium (days 3–6).
Surface epithelium is intact. Glands are straight and tubular without
mitotic figures or pseudostratification. This normal endometrium was exposed
only to estrogen stimulation at the time of biopsy. B. Late secretory
endometrium (days 25–26) in a normal menstrual cycle. Tissue has
been predominantly stimulated by progesterone for 11 to 12 days. Glands
are convoluted and have expended most of their secretory products. The
stroma has undergone an extensive decidual reaction.
A. Early proliferative endometrium (days 3–6).
Surface epithelium is intact. Glands are straight and tubular without
mitotic figures or pseudostratification. This normal endometrium was exposed
only to estrogen stimulation at the time of biopsy. B. Late secretory
endometrium (days 25–26) in a normal menstrual cycle. Tissue has
been predominantly stimulated by progesterone for 11 to 12 days. Glands
are convoluted and have expended most of their secretory products. The
stroma has undergone an extensive decidual reaction.
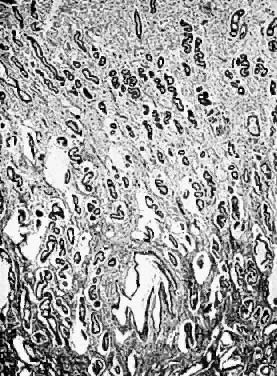
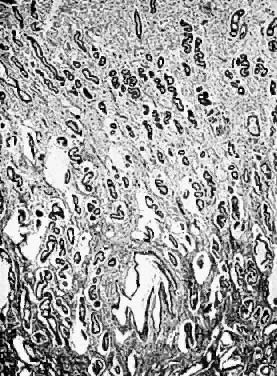
 Normal endometrial glands of uterus (resting
stage). Note the character of the epithelial cells of the glands; they
are slightly higher than the ciliated columnar cells of the surface epithelium.
There is a distinct basement membrane.
Normal endometrial glands of uterus (resting
stage). Note the character of the epithelial cells of the glands; they
are slightly higher than the ciliated columnar cells of the surface epithelium.
There is a distinct basement membrane.
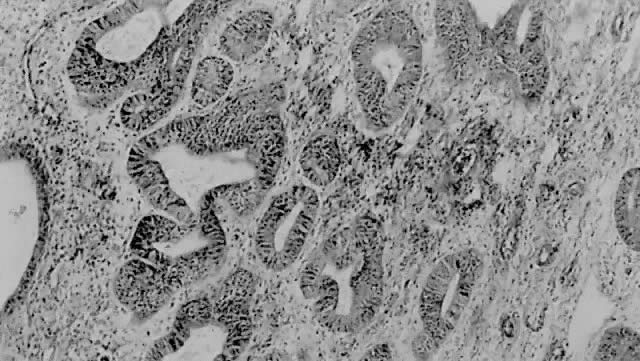
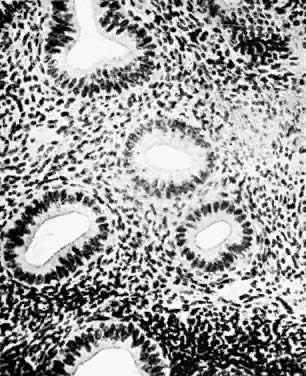
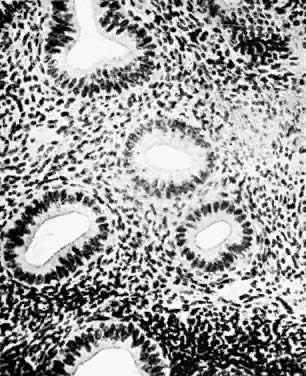
 Endometrium in the premenstrual stage. Note
that the glands are apparently increased in number and size. The tortuosity
of the glands is clearly seen.
Endometrium in the premenstrual stage. Note
that the glands are apparently increased in number and size. The tortuosity
of the glands is clearly seen.
Back to Top
Leiomyoma
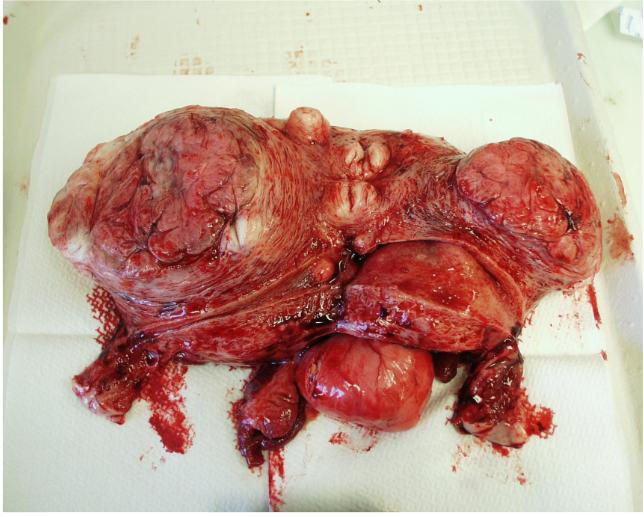
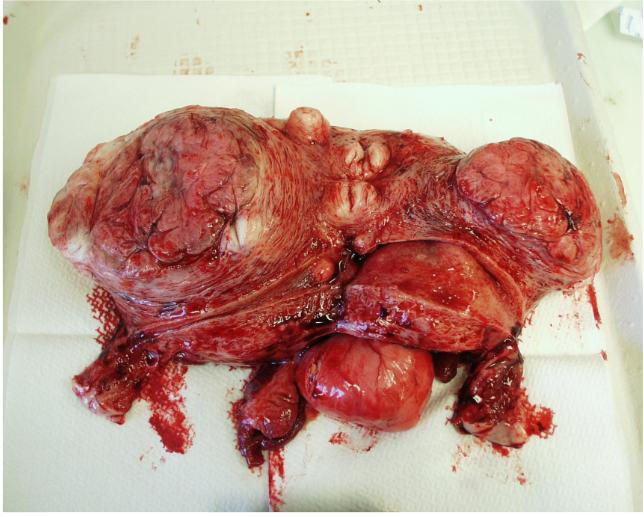 Multiple uterine fibroid tumors (Reproduced, with permission
from Michael John Hughey, MD, All rights reserved.)
Multiple uterine fibroid tumors (Reproduced, with permission
from Michael John Hughey, MD, All rights reserved.)
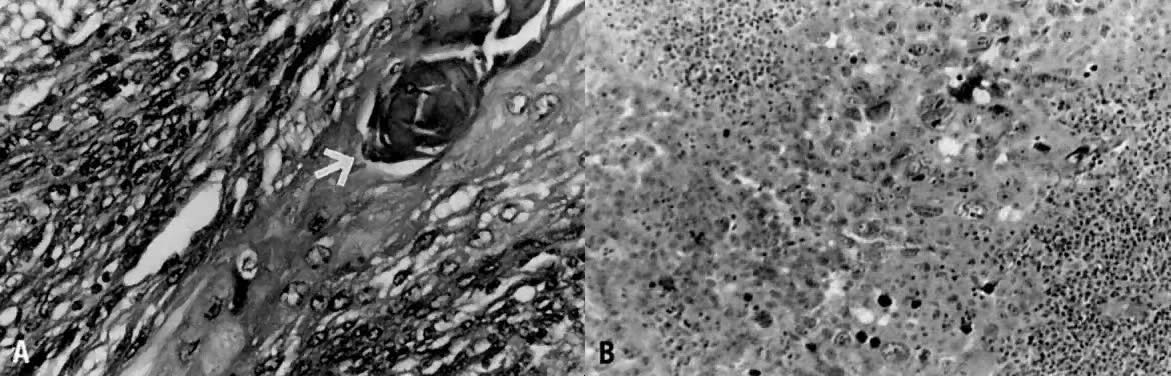
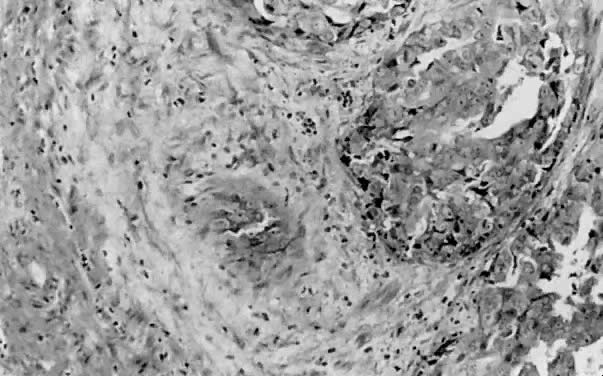
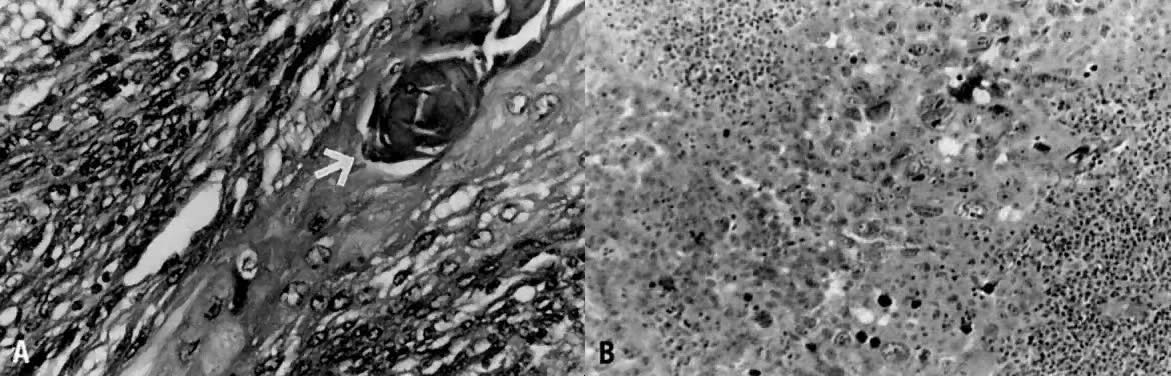
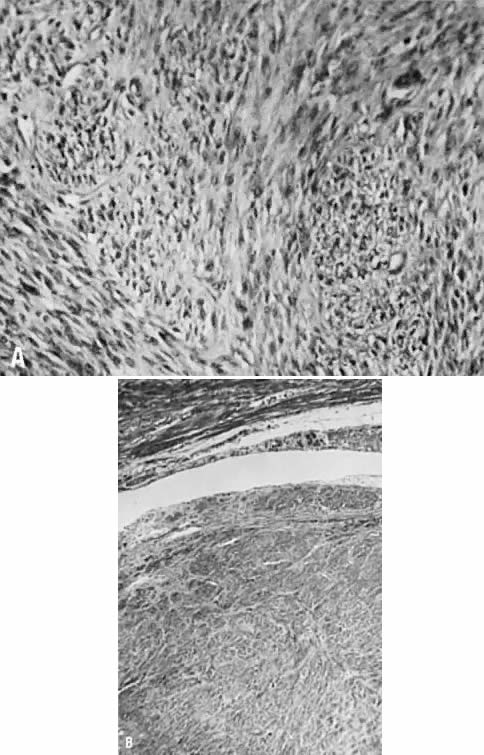 A. Intramural leiomyoma with whorled arrangement
of smooth muscle cells on a matrix of connective tissue cells (×200).
B. Notice the absence of distinct connective tissue capsule (×175).
( A and B, 66% of original magnification.)
A. Intramural leiomyoma with whorled arrangement
of smooth muscle cells on a matrix of connective tissue cells (×200).
B. Notice the absence of distinct connective tissue capsule (×175).
( A and B, 66% of original magnification.)
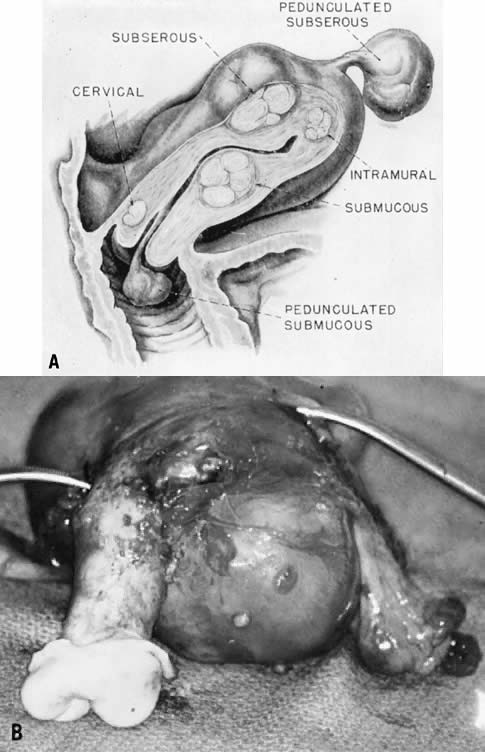
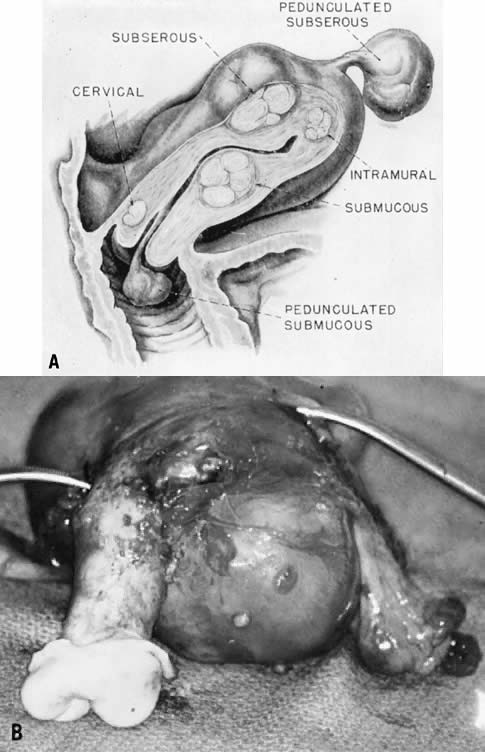 A. Uterine leiomyomas occupy various segments
of the uterus and various depths inside and outside the myometrium, and
they are designated by gross anatomic location. B. Fresh operative specimen
of a uterus was removed for multiple uterine leiomyomas.
A. Uterine leiomyomas occupy various segments
of the uterus and various depths inside and outside the myometrium, and
they are designated by gross anatomic location. B. Fresh operative specimen
of a uterus was removed for multiple uterine leiomyomas.
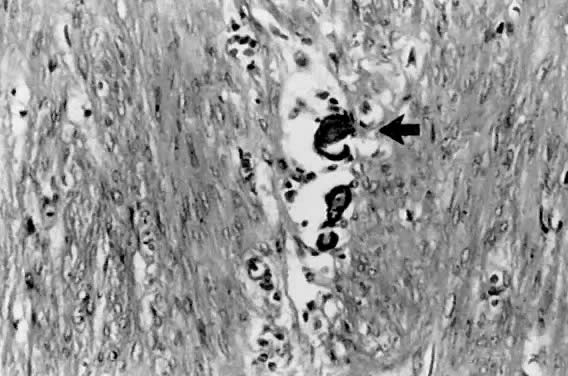
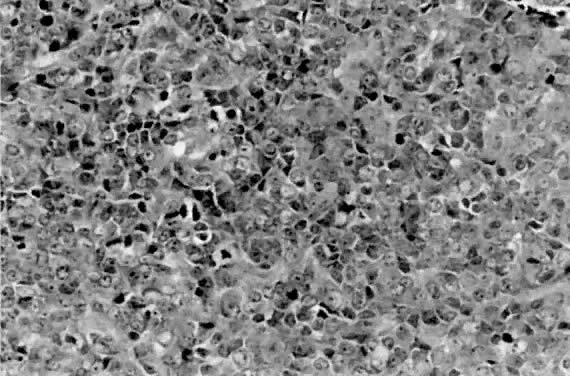
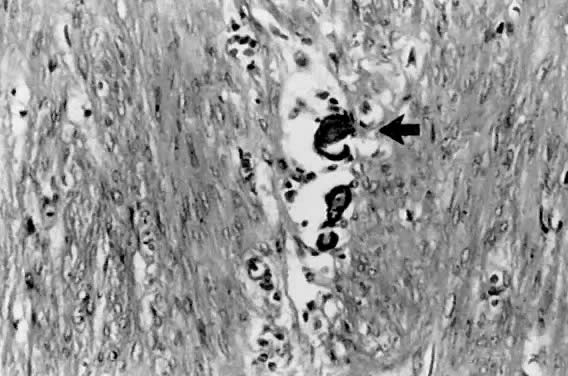
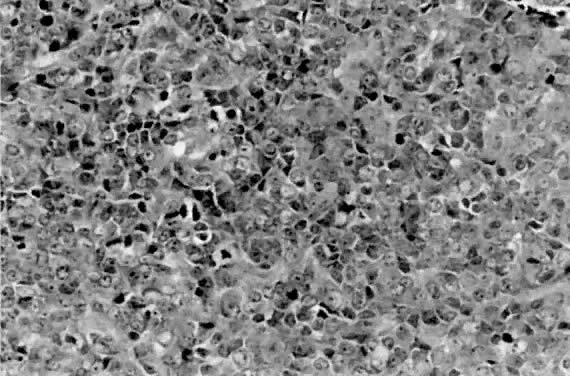
 Cellular leiomyoma with closely arranged smooth
muscle nuclei. An occasional mitotic figure is present (H&E, ×
90)
Cellular leiomyoma with closely arranged smooth
muscle nuclei. An occasional mitotic figure is present (H&E, ×
90)
Back to Top
Endometriosis
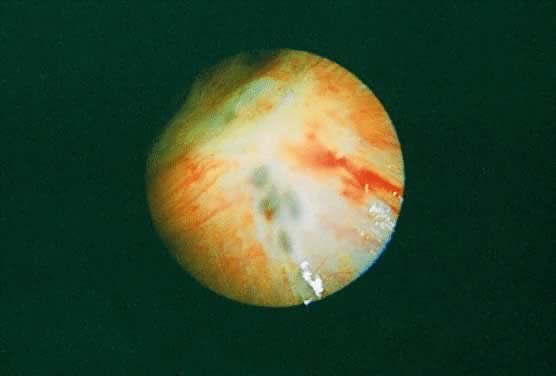
 Endometriosis
(From Operational Obstetrics & Gynecology - 2nd Edition, The Health
Care of Women in Military Settings, CAPT Michael John Hughey, MC, USNR,
NAVMEDPUB 6300-2C, Bureau of Medicine and Surgery, Department of the Navy,
2300 E Street NW, Washington, D.C. 20372-5300, January 1, 2000. Original
image courtesy CAPT Richard Stock, MC, USN) Endometriosis
(From Operational Obstetrics & Gynecology - 2nd Edition, The Health
Care of Women in Military Settings, CAPT Michael John Hughey, MC, USNR,
NAVMEDPUB 6300-2C, Bureau of Medicine and Surgery, Department of the Navy,
2300 E Street NW, Washington, D.C. 20372-5300, January 1, 2000. Original
image courtesy CAPT Richard Stock, MC, USN)
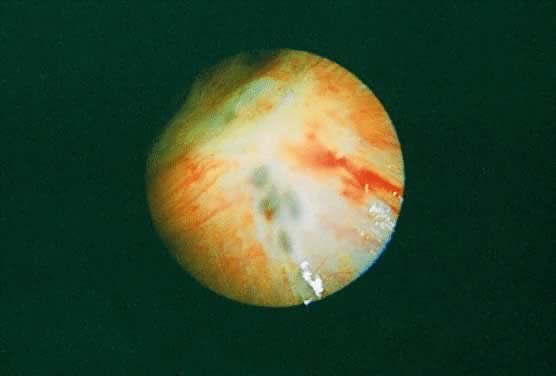 Characteristic "powder burn" appearance
of endometriosis implants located on the pelvic peritoneum.
Characteristic "powder burn" appearance
of endometriosis implants located on the pelvic peritoneum.
 Endometriosis implants in the cul-de-sac exhibit
multiple vesicles, “powder burn” lesions, and mild fibrosis.
Endometriosis implants in the cul-de-sac exhibit
multiple vesicles, “powder burn” lesions, and mild fibrosis.
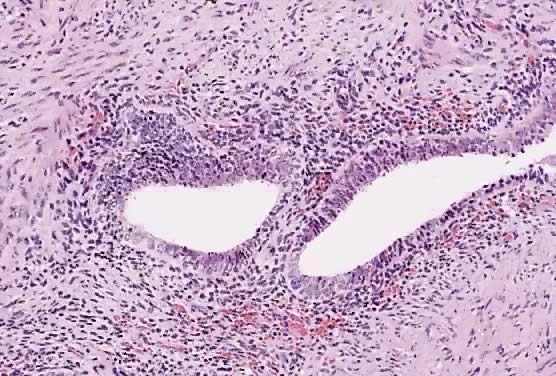
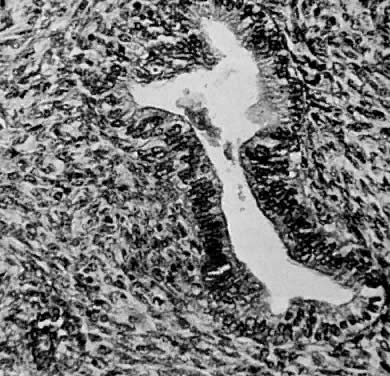
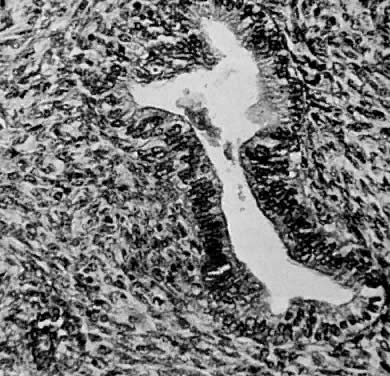
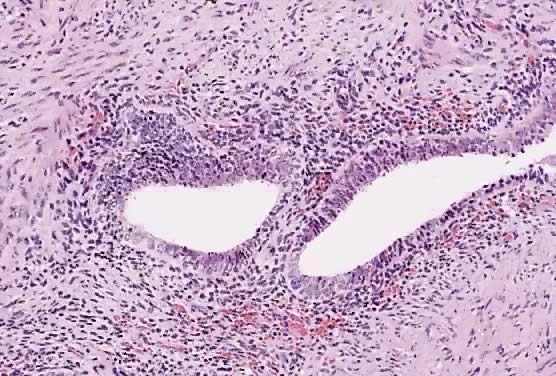 Pelvic peritoneal biopsy shows characteristic
features of endometriosis, with endometrioid glands surrounded by stroma
(hematoxylin and eosin stain, original magnification ×200).(Courtesy
of Mahendra Ranchod, M.D., Good Samaritan Hospital, San Jose, CA.)
Pelvic peritoneal biopsy shows characteristic
features of endometriosis, with endometrioid glands surrounded by stroma
(hematoxylin and eosin stain, original magnification ×200).(Courtesy
of Mahendra Ranchod, M.D., Good Samaritan Hospital, San Jose, CA.)
Back to Top
Tuberculous Endometritis
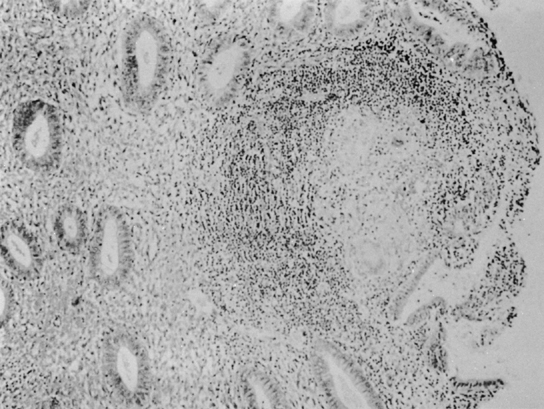
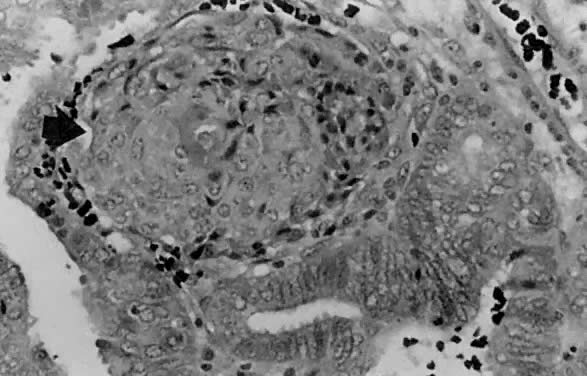
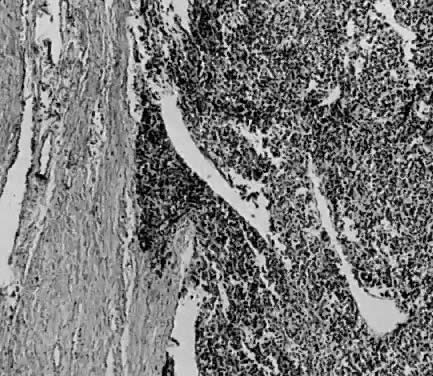
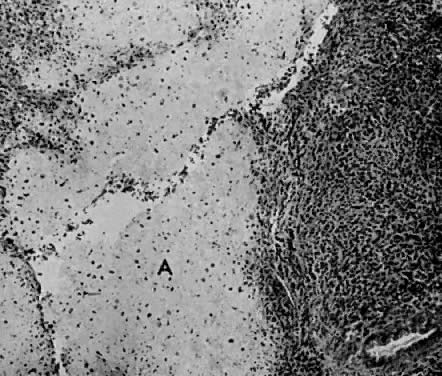
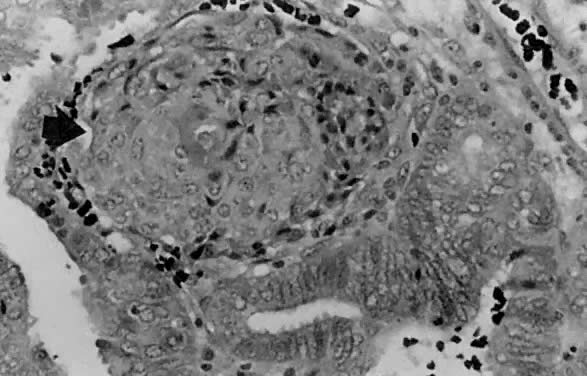
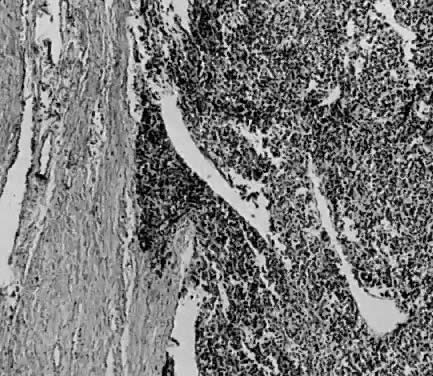
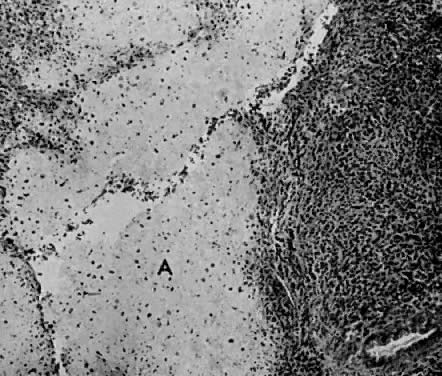
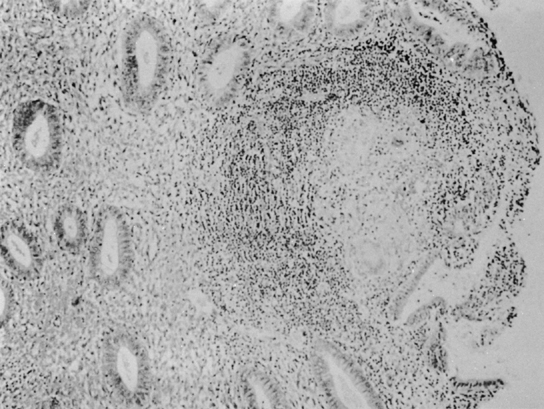 Tuberculous endometritis. Photomicrograph of
a single tuberculous granuloma is seen on the left, consisting of central
epithelioid cells, with a Langerhans-type giant cell surrounded by a cuff
of lymphocytes. No central caseation is present. The surrounding endometrium
appears completely normal; the glands are proliferative, and there is
no infiltrate in the stroma, seen on the right.(×100.)
Tuberculous endometritis. Photomicrograph of
a single tuberculous granuloma is seen on the left, consisting of central
epithelioid cells, with a Langerhans-type giant cell surrounded by a cuff
of lymphocytes. No central caseation is present. The surrounding endometrium
appears completely normal; the glands are proliferative, and there is
no infiltrate in the stroma, seen on the right.(×100.)
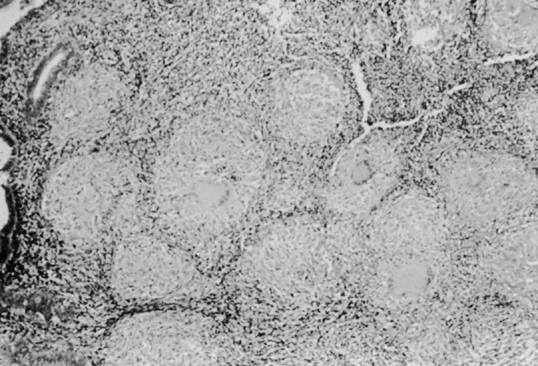
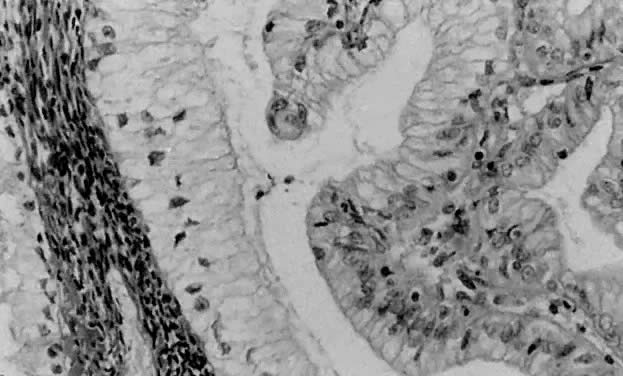
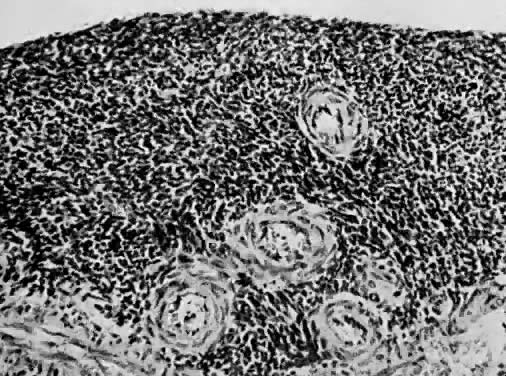
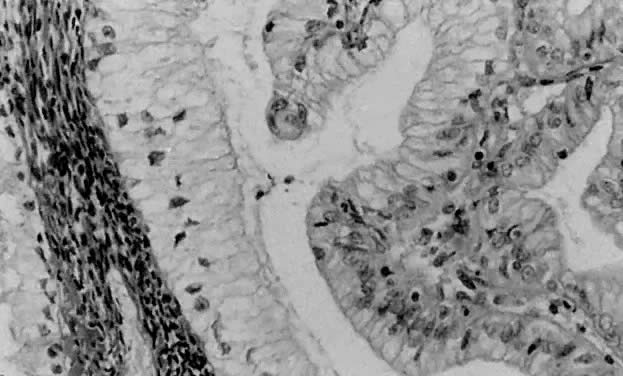
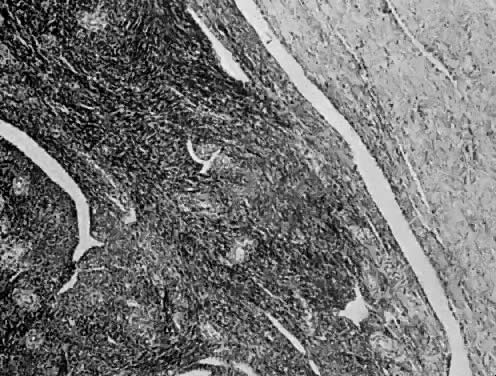
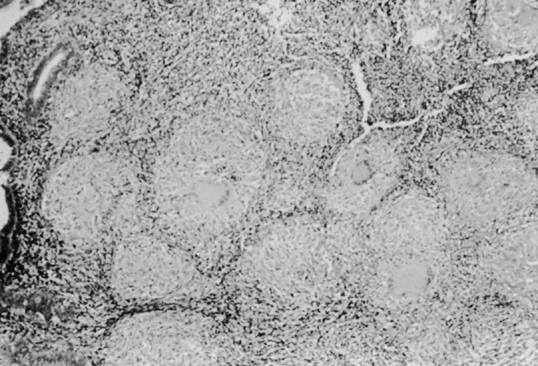 Tuberculous endometrium. A much more florid
picture of numerous granulomata with dense lymphocyte infiltrate in the
surrounding stroma is seen in this photomicrograph.(×100.)
Tuberculous endometrium. A much more florid
picture of numerous granulomata with dense lymphocyte infiltrate in the
surrounding stroma is seen in this photomicrograph.(×100.)
Back to Top
Arias-Stella Phenomenon
 Arias-Stella phenomenon.
Arias-Stella phenomenon.
Back to Top
Tubal Metaplasia
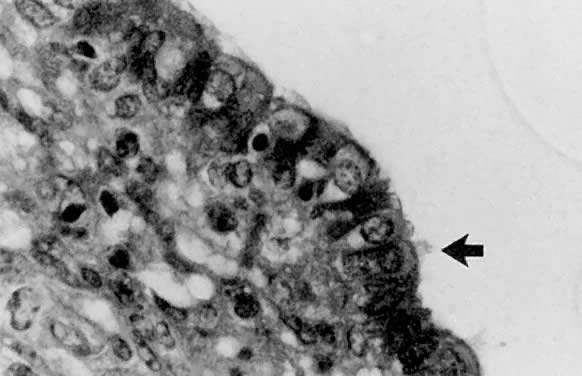
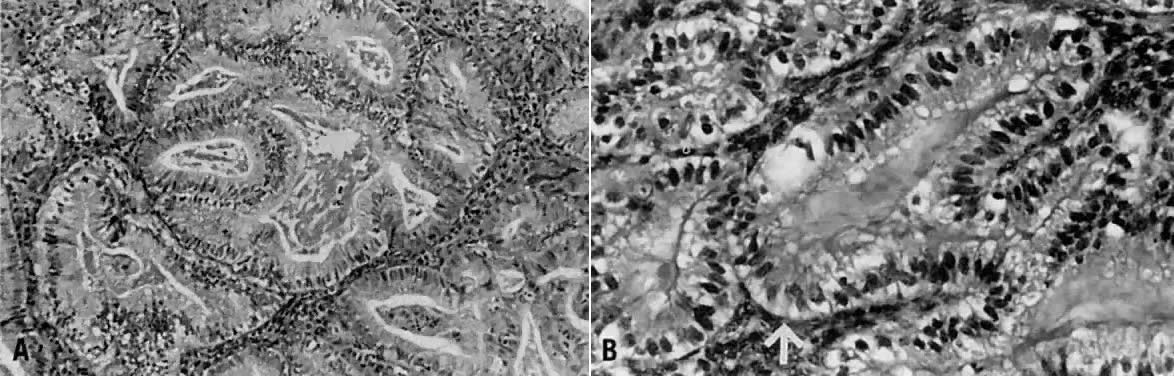
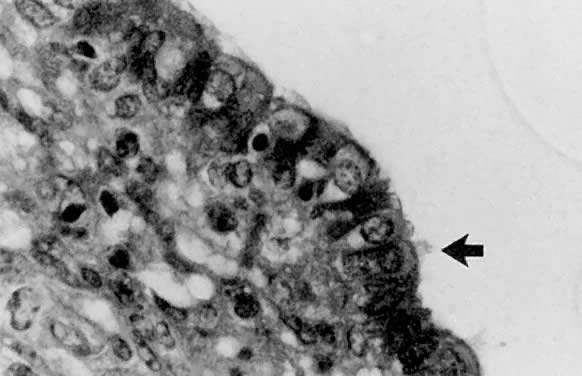 Tubal metaplasia is probably the most frequently
encountered metaplasia of the endometrium. Ciliated cells ( arrow) interdigitate
with peg cells, which have perinuclear clearing.
Tubal metaplasia is probably the most frequently
encountered metaplasia of the endometrium. Ciliated cells ( arrow) interdigitate
with peg cells, which have perinuclear clearing.
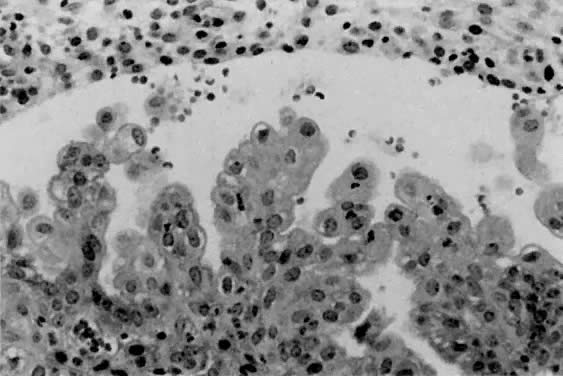
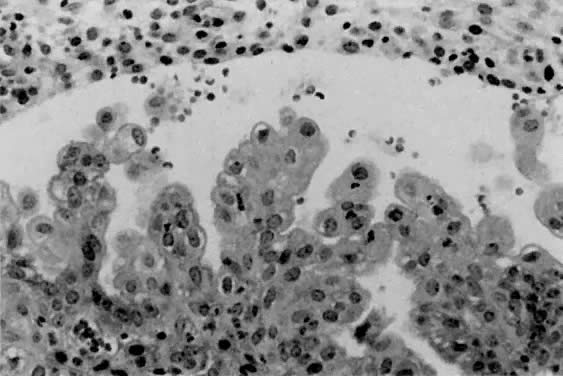 Papillary metaplasia may mimic an adenocarcinoma
with papillary features at low magnification; however, the bland, uniform
lining cells favor a benign process. Also, the papillae in papillary metaplasia
are limited to the surface epithelium.
Papillary metaplasia may mimic an adenocarcinoma
with papillary features at low magnification; however, the bland, uniform
lining cells favor a benign process. Also, the papillae in papillary metaplasia
are limited to the surface epithelium.
Back to Top
Endometrial Hyperplasia
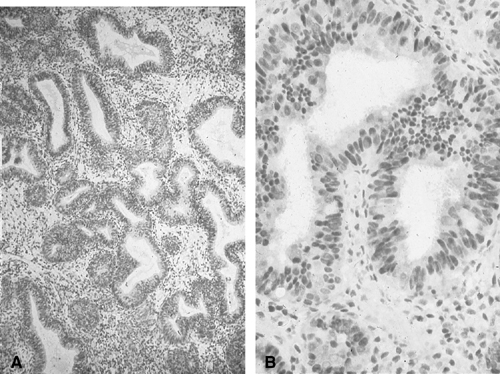
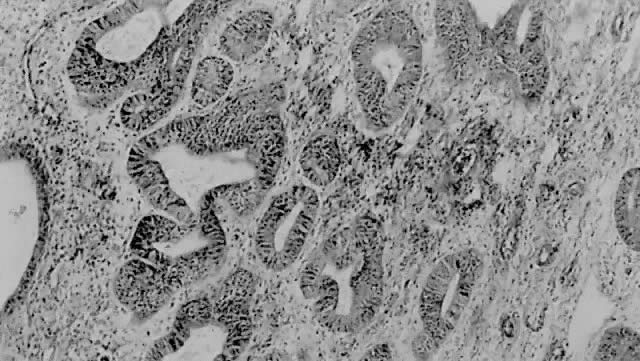
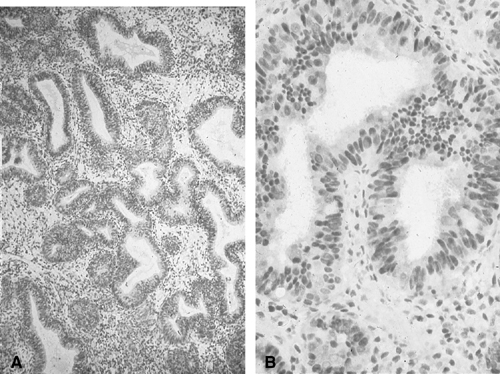 Histology of endometrial hyperplasia (without
atypia). A. Voluminous proliferative-type glands and abundant stroma.
B. Higher power magnification of tall, columnar gland cells with regular
nuclear pseudostratification and abundant intranuclear receptors for estrogen.
There is an increased number of crowded and irregularly shaped glands
relative to stroma.
Histology of endometrial hyperplasia (without
atypia). A. Voluminous proliferative-type glands and abundant stroma.
B. Higher power magnification of tall, columnar gland cells with regular
nuclear pseudostratification and abundant intranuclear receptors for estrogen.
There is an increased number of crowded and irregularly shaped glands
relative to stroma.
 Histology of endometrial intraepithelial neoplasia
(atypical hyperplasia). A. Voluminous gland with multiple intraluminal
microlumens (cribriform pattern). The lining epithelium has pleomorphic,
round nuclei devoid of regular pseudostratification. Macronucleoli are
present. B. High magnification of hyperplastic (left) and neoplastic (right)
epithelium. Note regular, nuclear pseudostratification of tall columnar
gland lining epithelium in hyperplasia without atypia. Endometrial intraepithelial
neoplasia (atypical hyperplasoa) has pleomorphic, round nuclei with macronucleoli,
and nuclear pseudostratification is lost.
Histology of endometrial intraepithelial neoplasia
(atypical hyperplasia). A. Voluminous gland with multiple intraluminal
microlumens (cribriform pattern). The lining epithelium has pleomorphic,
round nuclei devoid of regular pseudostratification. Macronucleoli are
present. B. High magnification of hyperplastic (left) and neoplastic (right)
epithelium. Note regular, nuclear pseudostratification of tall columnar
gland lining epithelium in hyperplasia without atypia. Endometrial intraepithelial
neoplasia (atypical hyperplasoa) has pleomorphic, round nuclei with macronucleoli,
and nuclear pseudostratification is lost.
 Although the endometrial glands within this
focus of complex hyperplasia are irregular and complex in configuration,
intervening stroma is present between the glands. This feature is important
in distinguishing complex hyperplasia from a well-differentiated adenocarcinoma.
Although the endometrial glands within this
focus of complex hyperplasia are irregular and complex in configuration,
intervening stroma is present between the glands. This feature is important
in distinguishing complex hyperplasia from a well-differentiated adenocarcinoma.
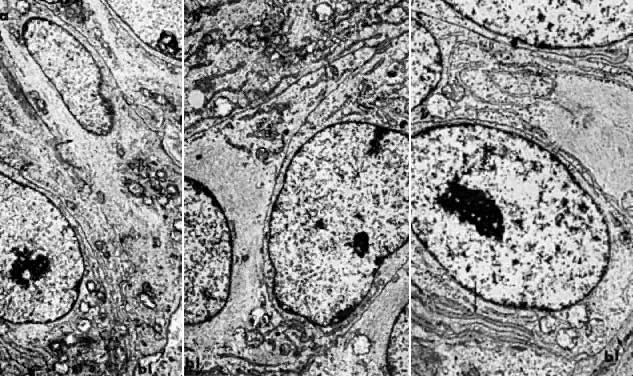
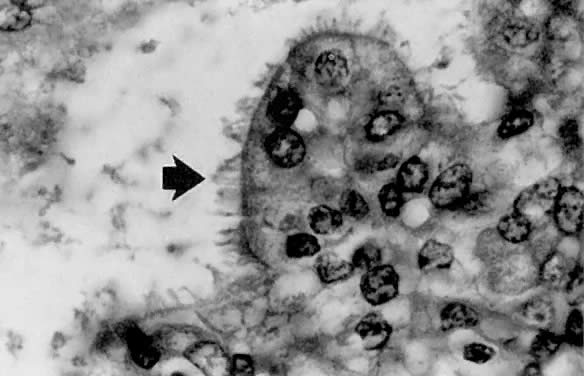
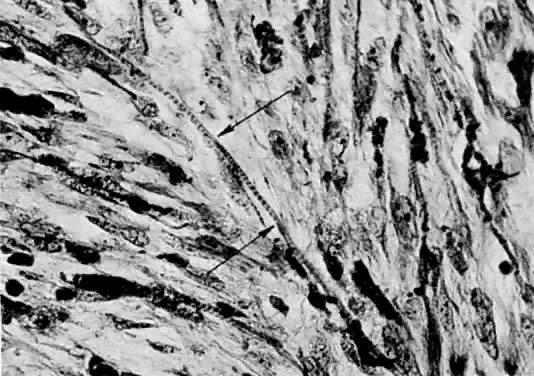
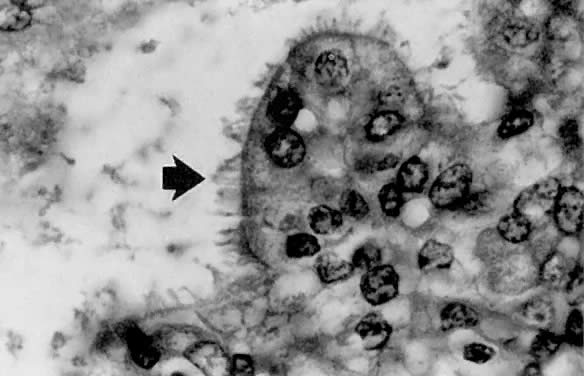
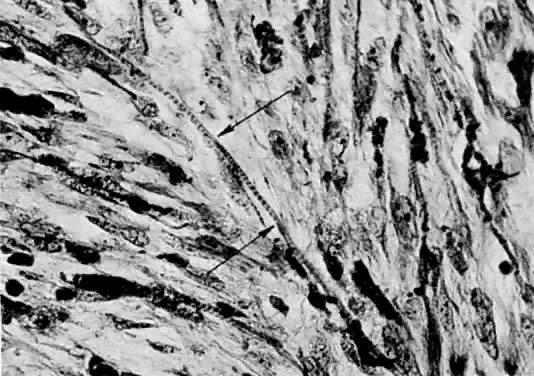
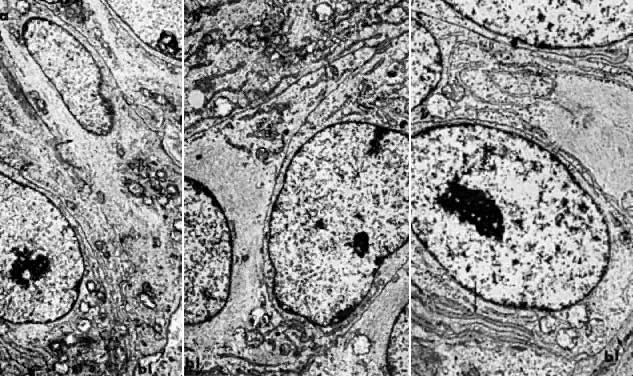 A. Adenomatous hyperplasia of the endometrium.
The basal portion of gland lining cells is shown. Note spindle-shaped
configuration of nuclei, abundant and narrow bundles of microfilaments
( arrow) extending to the supranuclear region, and monomorphic mitochondria
in close association with membranes of granular endoplasmic reticulum
(
A. Adenomatous hyperplasia of the endometrium.
The basal portion of gland lining cells is shown. Note spindle-shaped
configuration of nuclei, abundant and narrow bundles of microfilaments
( arrow) extending to the supranuclear region, and monomorphic mitochondria
in close association with membranes of granular endoplasmic reticulum
( 7000).
B. Carcinoma in situ of the endometrium. Note nuclear rounding, pleomorphic
organelles, and interlacing bundles of microfilaments in a perinuclear
location ( 7000).
B. Carcinoma in situ of the endometrium. Note nuclear rounding, pleomorphic
organelles, and interlacing bundles of microfilaments in a perinuclear
location ( 8000).
C. Well-differentiated, invasive adenocarcinoma of the endometrium. The
ultrastructural features are essentially similar to those found in carcinoma
in situ cells. The lateral plasma membranes ( arrow) and granular endoplasmic
reticulum are more convoluted than in carcinoma in situ cells ( 8000).
C. Well-differentiated, invasive adenocarcinoma of the endometrium. The
ultrastructural features are essentially similar to those found in carcinoma
in situ cells. The lateral plasma membranes ( arrow) and granular endoplasmic
reticulum are more convoluted than in carcinoma in situ cells ( 8000;
bl, basal lamina).(Courtesy of Alex Ferenczy) 8000;
bl, basal lamina).(Courtesy of Alex Ferenczy)
Back to Top
Adenocarcinoma
 A well-differentiated endometrioid adenocarcinoma
obtained from a curettage specimen. Note the absence of intervening stroma
between the irregularly shaped glands. Nuclei demonstrate only mild pleomorphism.
A well-differentiated endometrioid adenocarcinoma
obtained from a curettage specimen. Note the absence of intervening stroma
between the irregularly shaped glands. Nuclei demonstrate only mild pleomorphism.
 Contrast the marked nuclear pleomorphism and
solid growth pattern of this grade 3 endometrioid adenocarcinoma with
the well-differentiated carcinoma in
Contrast the marked nuclear pleomorphism and
solid growth pattern of this grade 3 endometrioid adenocarcinoma with
the well-differentiated carcinoma in
 The altered stroma adjacent to the invasive
foci of this high-grade endometrioid carcinoma is characteristic of a
desmoplastic stromal response. The pale staining is due to edema and myxoid
change, which is often accompanied by an inflammatory cell infiltrate.
The altered stroma adjacent to the invasive
foci of this high-grade endometrioid carcinoma is characteristic of a
desmoplastic stromal response. The pale staining is due to edema and myxoid
change, which is often accompanied by an inflammatory cell infiltrate.
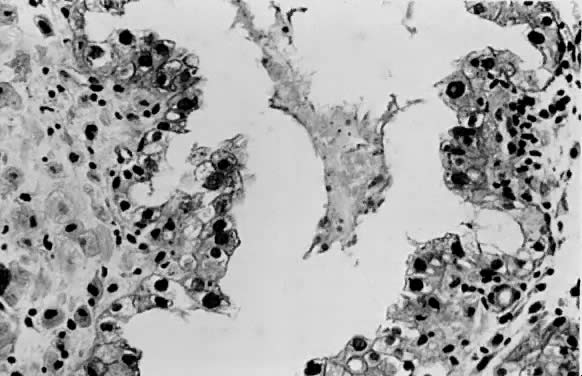
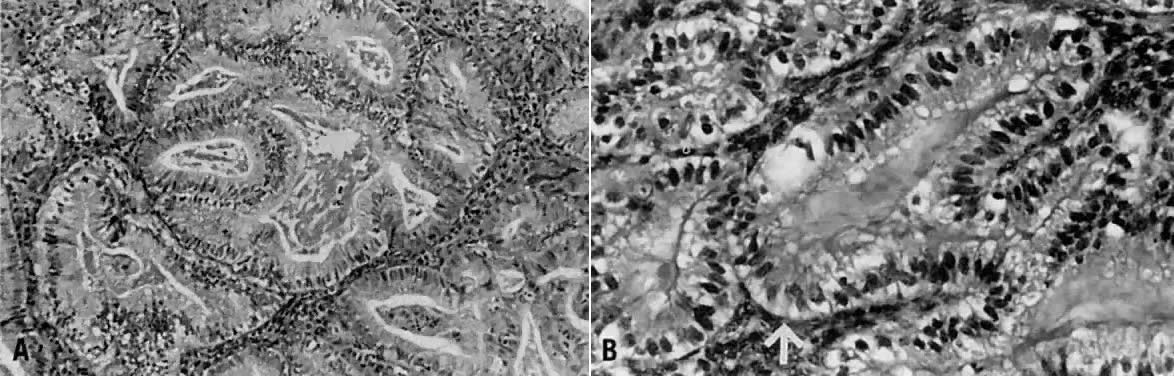
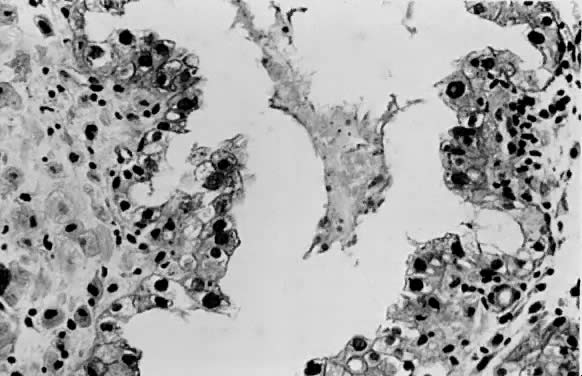
 ( A) Secretory carcinoma is characterized by
prominent cytoplasmic vacuoles and intraluminal secretions. ( B) The arrow
denotes the uniform subnuclear vacuoles.
( A) Secretory carcinoma is characterized by
prominent cytoplasmic vacuoles and intraluminal secretions. ( B) The arrow
denotes the uniform subnuclear vacuoles.
 Ciliated cell carcinoma. Most of the neoplastic
glands are lined by ciliated cells ( arrow) showing mild to moderate nuclear
atypia.
Ciliated cell carcinoma. Most of the neoplastic
glands are lined by ciliated cells ( arrow) showing mild to moderate nuclear
atypia.
 Squamous differentiation in endometrial adenocarcinoma
is frequent. This is an example of a squamous morule ( arrow ), which
is a collection of polygonal cells with abundant eosinophilic cytoplasm
forming a nodular structure between neoplastic endometrial glands.
Squamous differentiation in endometrial adenocarcinoma
is frequent. This is an example of a squamous morule ( arrow ), which
is a collection of polygonal cells with abundant eosinophilic cytoplasm
forming a nodular structure between neoplastic endometrial glands.
 Mucinous carcinoma is generally well differentiated
and is characterized by columnar cells with basally located nuclei and
mucin-rich cytoplasm.
Mucinous carcinoma is generally well differentiated
and is characterized by columnar cells with basally located nuclei and
mucin-rich cytoplasm.
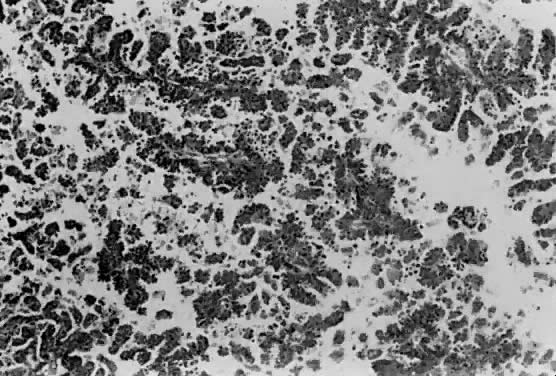
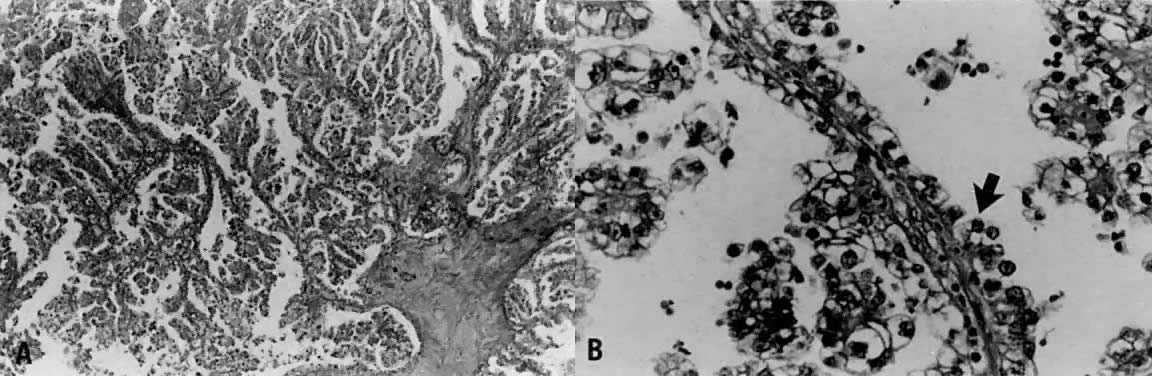
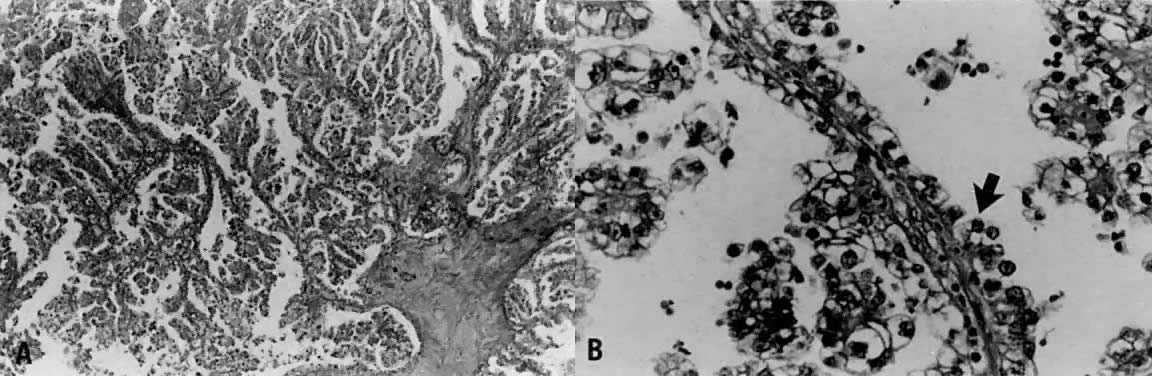
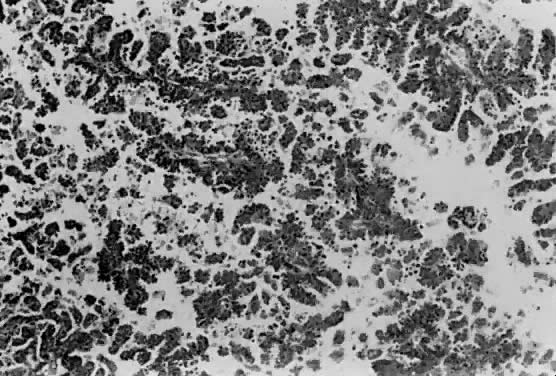 Complex arborization of papillary structures
is seen in serous carcinoma. Cellular budding and tufting can often be
appreciated under low power.
Complex arborization of papillary structures
is seen in serous carcinoma. Cellular budding and tufting can often be
appreciated under low power.
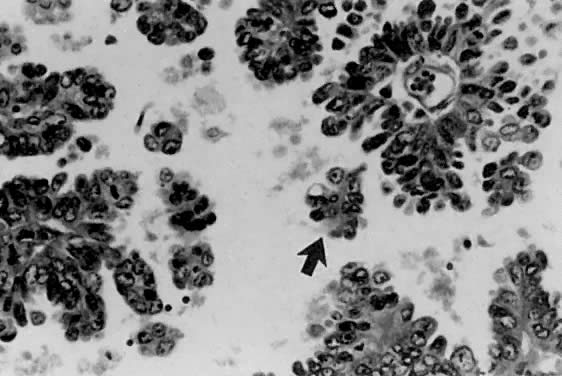
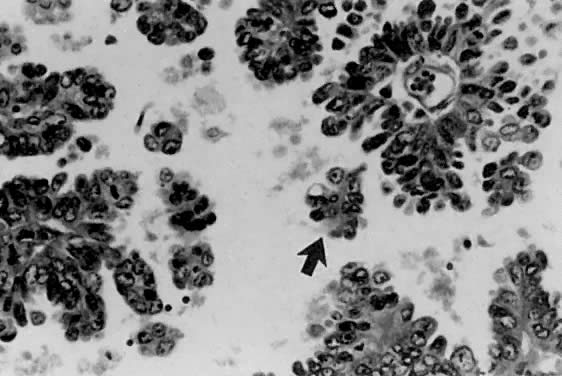 Serous carcinoma. The papillae have fibrovascular
cores and are lined by vesicular nuclei with prominent eosinophilic nucleoli.
Small clusters of cells that have separated from the papillae are referred
to as cellular budding ( arrow ).
Serous carcinoma. The papillae have fibrovascular
cores and are lined by vesicular nuclei with prominent eosinophilic nucleoli.
Small clusters of cells that have separated from the papillae are referred
to as cellular budding ( arrow ).
 Although more commonly seen in serous carcinoma,
psammoma bodies ( arrow) may also be found in the villoglandular variant
of endometrial carcinoma.
Although more commonly seen in serous carcinoma,
psammoma bodies ( arrow) may also be found in the villoglandular variant
of endometrial carcinoma.
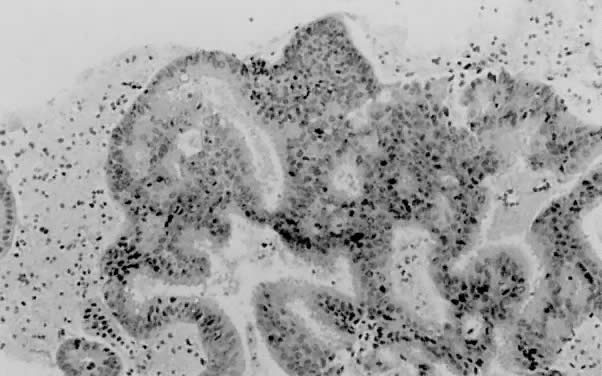
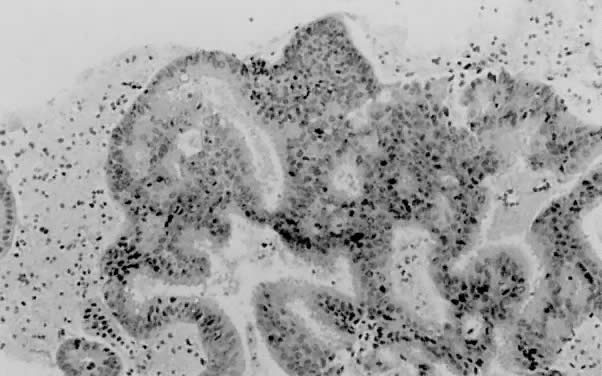
 A. Endometrial carcinoma, grade 1. A biopsy
specimen prior to the administration of progestogen. B. Endometrial biopsy
performed 8 weeks after commencement of 400 mg medroxyprogesterone three
times per week by intramuscular injection. C. The patient was treated
for 12 weeks with intramuscular medroxyprogesterone. Endometrium is shown
at the time of hysterectomy; no carcinomatous tissue is visible.
A. Endometrial carcinoma, grade 1. A biopsy
specimen prior to the administration of progestogen. B. Endometrial biopsy
performed 8 weeks after commencement of 400 mg medroxyprogesterone three
times per week by intramuscular injection. C. The patient was treated
for 12 weeks with intramuscular medroxyprogesterone. Endometrium is shown
at the time of hysterectomy; no carcinomatous tissue is visible.
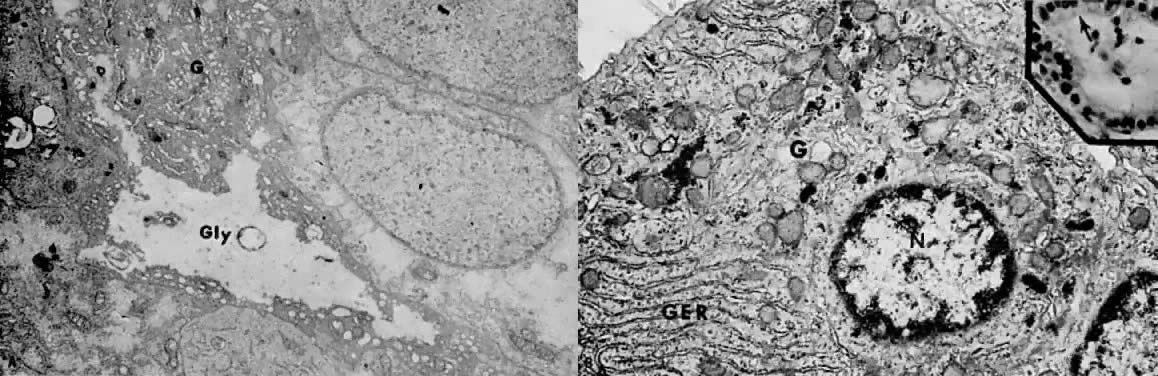
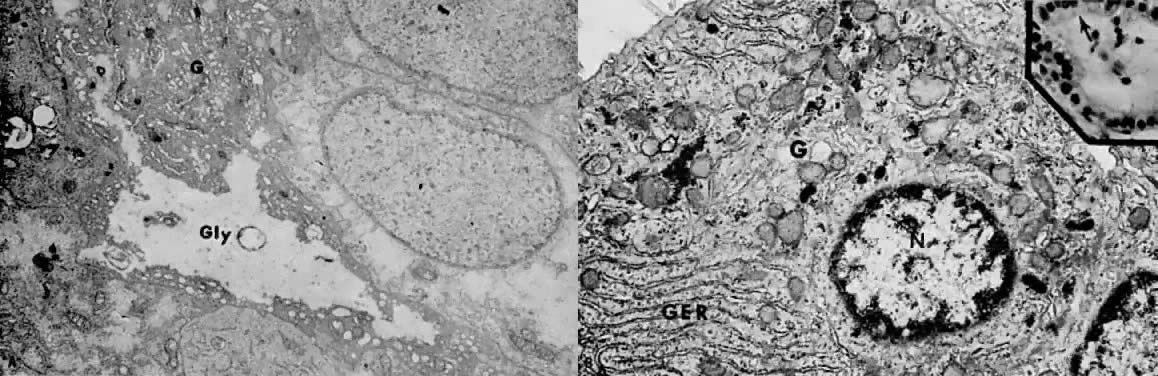 A. Well-differentiated adenocarcinoma 4 weeks
after treatment with medroxyprogesterone acetate. The early cellular effects
of progestin therapy include lack of nuclear chromatin clumping, regular
nuclear membranes, accumulation of large masses of intracytoplasmic glycogen
( Gly ), and hypertrophy of the Golgi complex ( G ). These features are
consistent with active synthesis of glycoproteins (
A. Well-differentiated adenocarcinoma 4 weeks
after treatment with medroxyprogesterone acetate. The early cellular effects
of progestin therapy include lack of nuclear chromatin clumping, regular
nuclear membranes, accumulation of large masses of intracytoplasmic glycogen
( Gly ), and hypertrophy of the Golgi complex ( G ). These features are
consistent with active synthesis of glycoproteins ( 5000).
(Courtesy of Alex Ferenczy) B. Moderately differentiated, invasive adenocarcinoma
90 days after treatment with medroxyprogesterone acetate. ( Inset) Following
secretory conversion and activity, the neoplastic cells appear reduced
in size (“exhausted”) and have supranuclear vacuoles ( arrow
). Note nuclear normochromasia and lack of nuclear pseudostratification
(H&E, 5000).
(Courtesy of Alex Ferenczy) B. Moderately differentiated, invasive adenocarcinoma
90 days after treatment with medroxyprogesterone acetate. ( Inset) Following
secretory conversion and activity, the neoplastic cells appear reduced
in size (“exhausted”) and have supranuclear vacuoles ( arrow
). Note nuclear normochromasia and lack of nuclear pseudostratification
(H&E,  350).
As a result of secretory differentiation, the granular endoplasmic reticulum
( GER ), mitochondria, and Golgi complex ( G) are hypertrophic. Owing
to secretion of glycogen-rich apical cytoplasmic substance, only minute
amounts of glycogen granules ( arrow) are found at this stage of therapy
( 350).
As a result of secretory differentiation, the granular endoplasmic reticulum
( GER ), mitochondria, and Golgi complex ( G) are hypertrophic. Owing
to secretion of glycogen-rich apical cytoplasmic substance, only minute
amounts of glycogen granules ( arrow) are found at this stage of therapy
( 27,000;
N, nucleus).(Courtesy of Alex Ferenczy) 27,000;
N, nucleus).(Courtesy of Alex Ferenczy)
Back to Top
Clear Cell Carcinoma
 ( A) This example of the papillary pattern
of clear cell carcinoma demonstrates complex papillae with fibrovascular
cores lined by one to multiple layers of clear cells. ( B) Hobnail cells
protrude into a cystic space ( arrow ). Other cells display the typical
clear cell morphology with irregular, primitive-appearing nuclei and abundant
clear cytoplasm that is rich in glycogen.
( A) This example of the papillary pattern
of clear cell carcinoma demonstrates complex papillae with fibrovascular
cores lined by one to multiple layers of clear cells. ( B) Hobnail cells
protrude into a cystic space ( arrow ). Other cells display the typical
clear cell morphology with irregular, primitive-appearing nuclei and abundant
clear cytoplasm that is rich in glycogen.
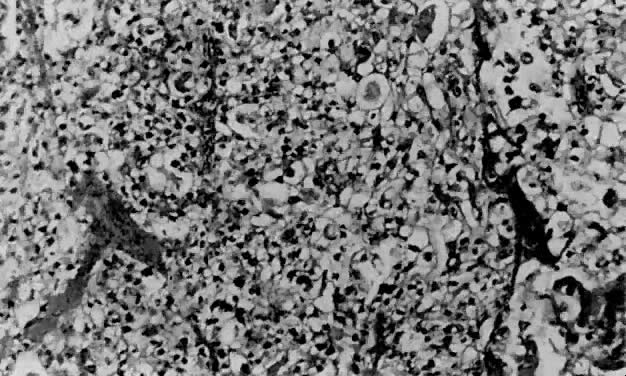
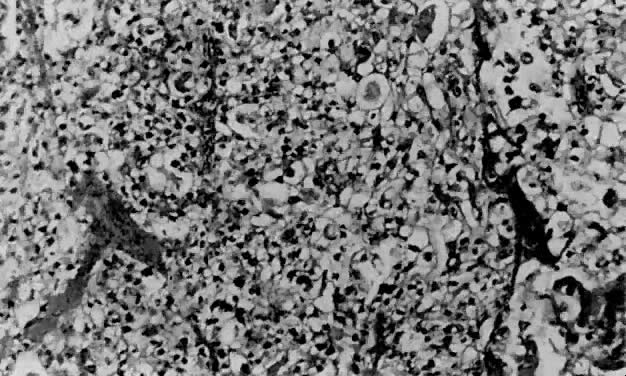 Clear cell carcinoma may exhibit a solid pattern
consisting of sheets of clear cells separated focally by thin fibrous
bands.
Clear cell carcinoma may exhibit a solid pattern
consisting of sheets of clear cells separated focally by thin fibrous
bands.
Back to Top
Squamous Cell Carcinoma
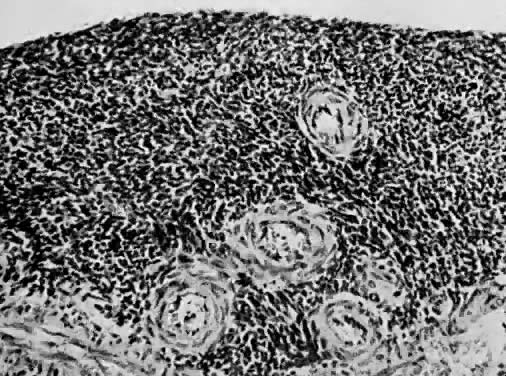
 ( A) As with squamous cell carcinoma in other
locations, the presence of keratin pearls ( arrow) or intercellular bridges
is diagnostic. ( B) The neoplastic cells have voluminous eosinophilic
cytoplasm and marked nuclear atypia.
( A) As with squamous cell carcinoma in other
locations, the presence of keratin pearls ( arrow) or intercellular bridges
is diagnostic. ( B) The neoplastic cells have voluminous eosinophilic
cytoplasm and marked nuclear atypia.
Back to Top
Small Cell Carcinoma
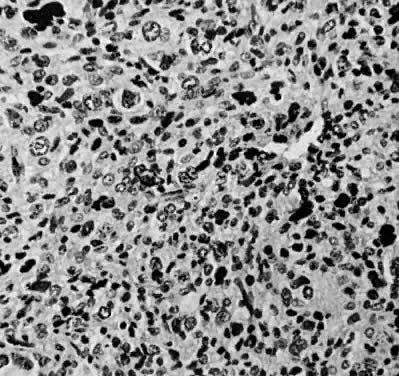
 Small cell carcinoma is characterized by sheets
of round to oval cells with granular chromatin and often dot-like nucleoli.
The mitotic rate is quite high in these clinically aggressive lesions.
Small cell carcinoma is characterized by sheets
of round to oval cells with granular chromatin and often dot-like nucleoli.
The mitotic rate is quite high in these clinically aggressive lesions.
Back to Top
Leiomyosarcoma
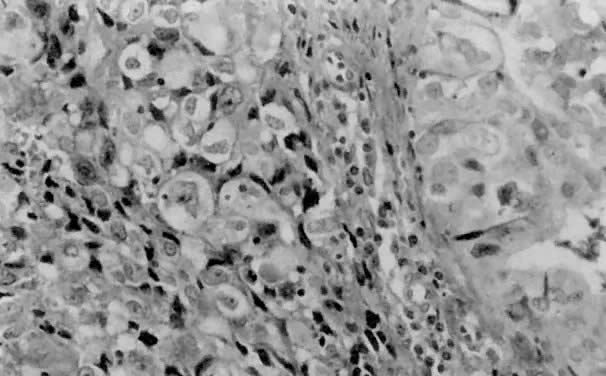
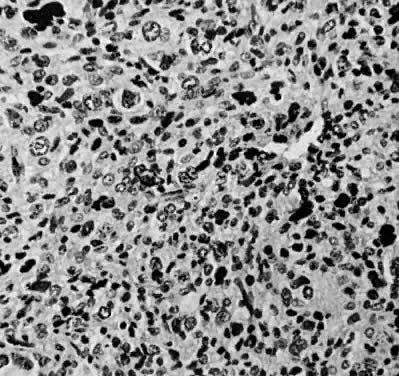
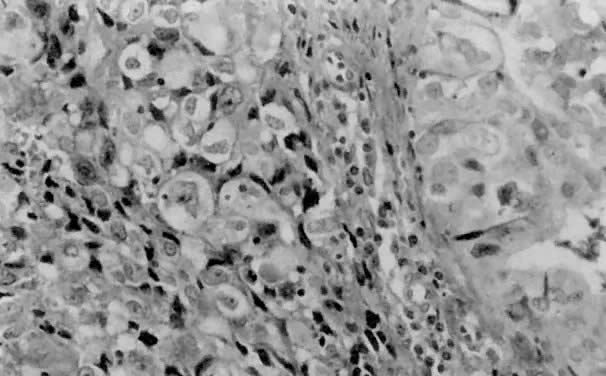
 Leiomyosarcoma displaying pleomorphism, giant
cells, and abnormal mitosis (H&E, × 350)
Leiomyosarcoma displaying pleomorphism, giant
cells, and abnormal mitosis (H&E, × 350)
Back to Top
Endometrial Stromal Sarcoma
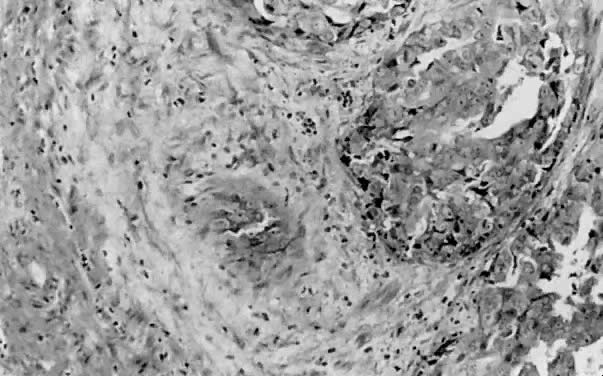
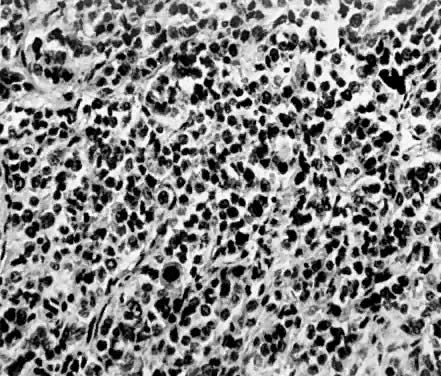
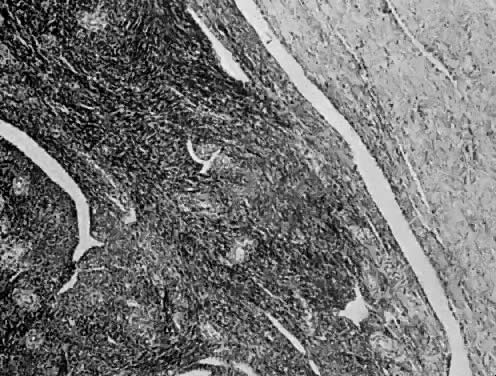
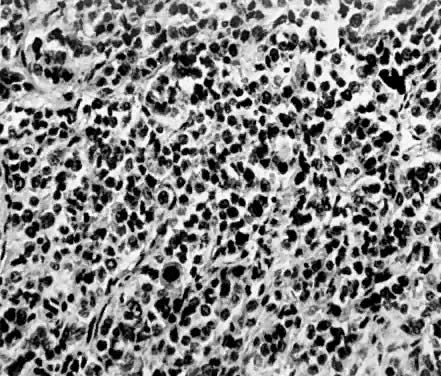 Endometrial stromal sarcoma composed of nests
of uniform cells with round nuclei separated by a delicate stroma. Several
abnormal mitoses are present (H&E, × 350)
Endometrial stromal sarcoma composed of nests
of uniform cells with round nuclei separated by a delicate stroma. Several
abnormal mitoses are present (H&E, × 350)
 Endometrial stromal sarcoma infiltrating between
muscle bundles (H&E, × 90)
Endometrial stromal sarcoma infiltrating between
muscle bundles (H&E, × 90)
Back to Top
Endolymphatic Stromal Myosis
 Cellular detail of endolymphatic stromal myosis.
The cells are uniform. There is minimal cellular atypia and no mitosis
(H&E, × 350)
Cellular detail of endolymphatic stromal myosis.
The cells are uniform. There is minimal cellular atypia and no mitosis
(H&E, × 350)
 Endolymphatic stromal myosis showing pushing
margin (H&E, × 90)
Endolymphatic stromal myosis showing pushing
margin (H&E, × 90)
Back to Top
Other Malignancies
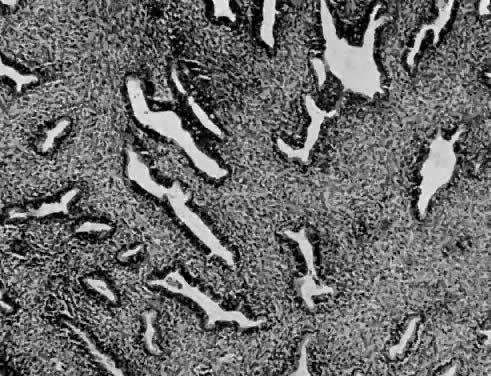
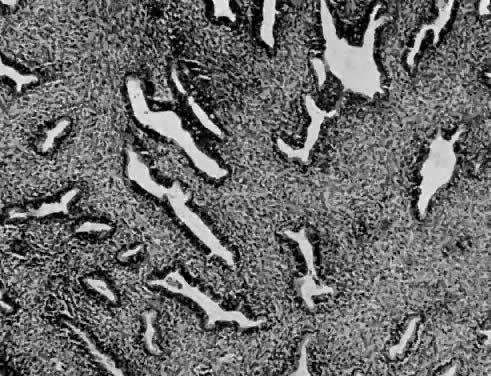 Müllerian adenosarcoma is composed of
branching endometrial glands lined by benign epithelium and surrounded
by malignant stroma (H&E, × 90)
Müllerian adenosarcoma is composed of
branching endometrial glands lined by benign epithelium and surrounded
by malignant stroma (H&E, × 90)
 Cellular detail of müllerian adenosarcoma.
The epithelium lining this endometrial gland appears benign; however,
the surrounding stromal cells are round to spindle shaped with several
mitotic figures present (H&E, × 350)
Cellular detail of müllerian adenosarcoma.
The epithelium lining this endometrial gland appears benign; however,
the surrounding stromal cells are round to spindle shaped with several
mitotic figures present (H&E, × 350)
 Rhabdomyosarcoma showing strap-shaped rhabdomyoblasts
( arrows) with cross-striations (× 600).
Rhabdomyosarcoma showing strap-shaped rhabdomyoblasts
( arrows) with cross-striations (× 600).
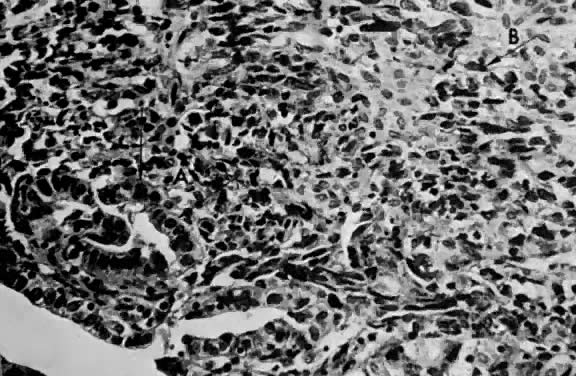
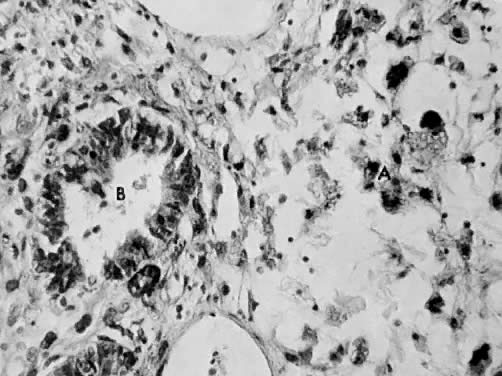
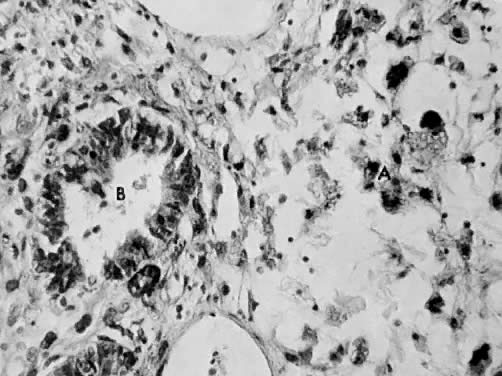
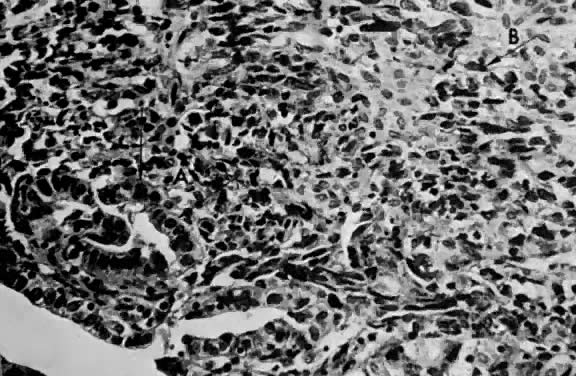 Mixed homologous mesodermal sarcoma showing
islands of adenocarcinoma ( A) scattered in a leiomyosarcomatous stroma
( B) (H&E, × 350) V
Mixed homologous mesodermal sarcoma showing
islands of adenocarcinoma ( A) scattered in a leiomyosarcomatous stroma
( B) (H&E, × 350) V
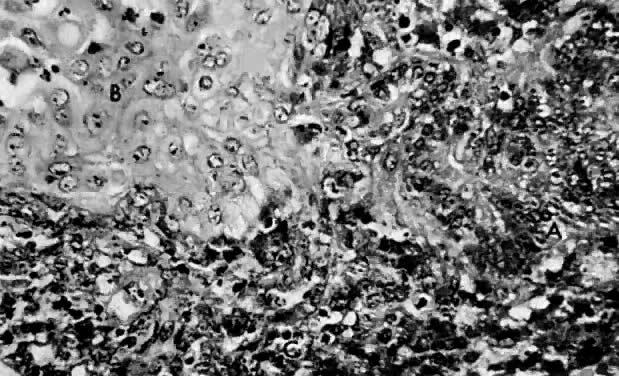
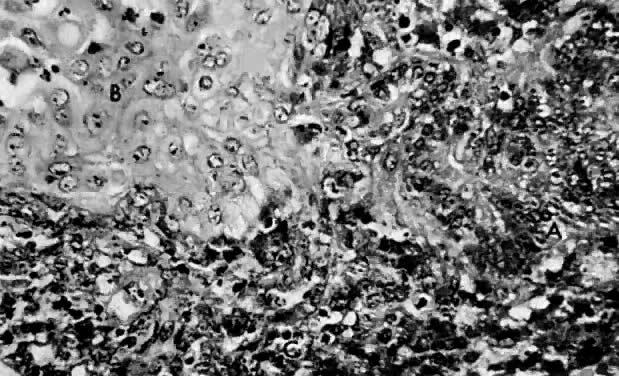 Mixed homologous mesodermal sarcoma composed
of islands of adenocarcinoma ( A) and squamous carcinoma ( B) with leiomyosarcoma
( C) (H&E, × 350)
Mixed homologous mesodermal sarcoma composed
of islands of adenocarcinoma ( A) and squamous carcinoma ( B) with leiomyosarcoma
( C) (H&E, × 350)
 Mixed heterologous mesodermal sarcoma showing
chondrosarcoma ( A) as the heterologous element (H&E, × 90)
Mixed heterologous mesodermal sarcoma showing
chondrosarcoma ( A) as the heterologous element (H&E, × 90)
 Mixed heterologous mesodermal sarcoma showing
osteogenic ( A) sarcoma as the heterologous component (H&E, ×
350)
Mixed heterologous mesodermal sarcoma showing
osteogenic ( A) sarcoma as the heterologous component (H&E, ×
350)
 Mixed heterologous mesodermal sarcoma showing
liposarcoma ( A) as the heterologous element of the neoplasm and adenocarcinoma
( B) (H&E, × 350)
Mixed heterologous mesodermal sarcoma showing
liposarcoma ( A) as the heterologous element of the neoplasm and adenocarcinoma
( B) (H&E, × 350)
Back to Top
| 

 Multiple uterine fibroid tumors (Reproduced, with permission
from Michael John Hughey, MD, All rights reserved.)
Multiple uterine fibroid tumors (Reproduced, with permission
from Michael John Hughey, MD, All rights reserved.)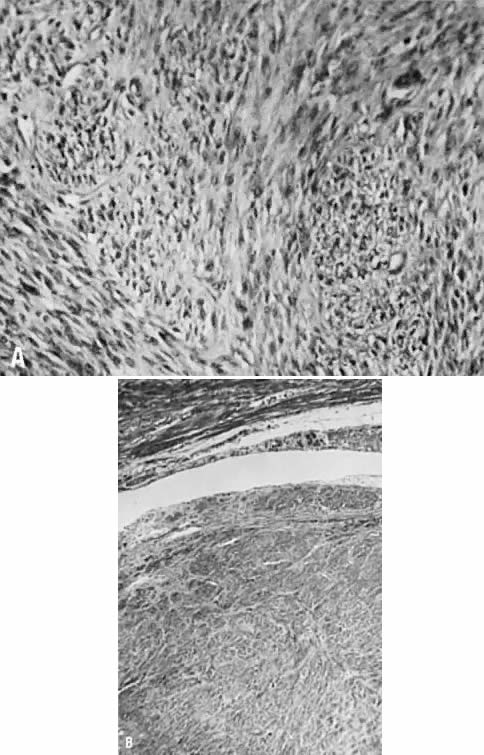

 Endometriosis
(From Operational Obstetrics & Gynecology - 2nd Edition, The Health
Care of Women in Military Settings, CAPT Michael John Hughey, MC, USNR,
NAVMEDPUB 6300-2C, Bureau of Medicine and Surgery, Department of the Navy,
2300 E Street NW, Washington, D.C. 20372-5300, January 1, 2000. Original
image courtesy CAPT Richard Stock, MC, USN)
Endometriosis
(From Operational Obstetrics & Gynecology - 2nd Edition, The Health
Care of Women in Military Settings, CAPT Michael John Hughey, MC, USNR,
NAVMEDPUB 6300-2C, Bureau of Medicine and Surgery, Department of the Navy,
2300 E Street NW, Washington, D.C. 20372-5300, January 1, 2000. Original
image courtesy CAPT Richard Stock, MC, USN)